
Moreover, we have the feeling that in real-life clinical
practice, the difference between the two approaches could be
more pronounced. First, the pragmatic feature of a single-
surgeon RCT might be a disadvantage for RSP. Indeed, Mani
Menon is one of themost experienced prostate cancer robotic
surgeons in the world, with several thousand cases treated
using the Vattikuti Institute Prostatectomy approach
[2], and
only 60 cases of RSP before the RCT. Second, the patients
included in the study are of only low and intermediate risk,
while the majority of patients with the risk of urinary
incontinence are those requiring wide anatomical dissection,
that is, those with high-risk prostate cancer
[3]. Third,
technical modifications might further improve the results
of this newborn technique (eg, we do not know the effects of
posterior reconstruction with this approach).
In 2010, our RSP experience also began with carefully
selected, low-risk cases
[4] .At that time, we assumed that
the patients who would gain the greatest advantage from
such a ‘‘conservative’’ approach were those deserving a
nerve-sparing surgery. However, after more than 1200 RSP
cases, we can affirm that the widest gap between RARP and
RSP can be seen in non–nerve-sparing cases.
Figure 1shows
the urinary continence results in our first 600 cases, divided
by nerve-sparing status. Extrafascial dissection exacerbates
the urinary continence results, which are nonetheless
superior to what everybody might expect from wide
demolition using standard RARP
[5] .In numerical terms,
70% of non–nerve-sparing patients can still be considered
continent (no pad/safety liner) 1 wk after surgery.
Unfortunately, ours are
nonpragmatic
data, with no control
arm, multiple surgeons, no blinded methodology, and no
pad weights.
These results pushed our group to use this approach even
in the most challenging cases: very large prostates, big
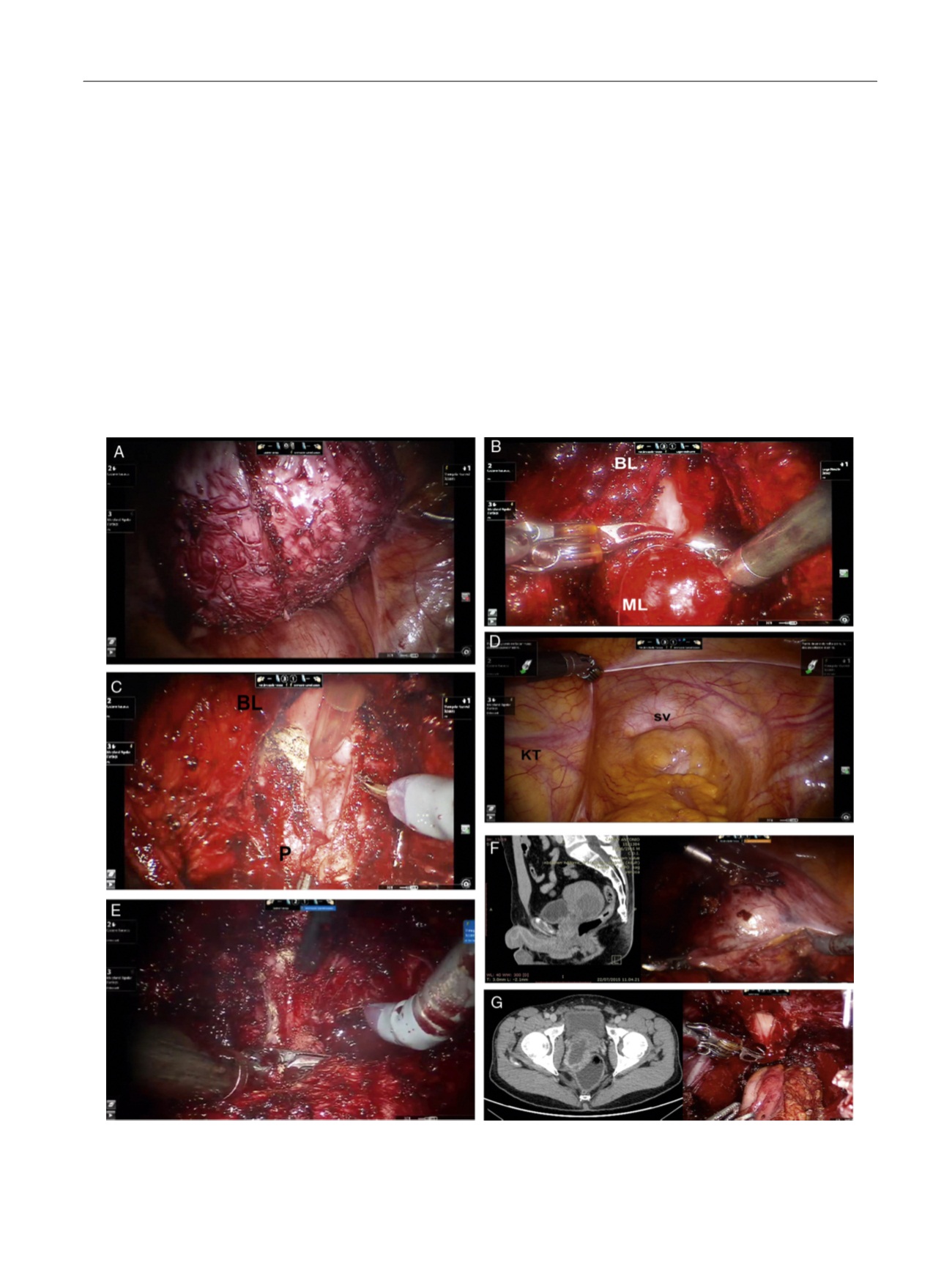
[(Fig._2)TD$FIG]
Fig. 2 – Challenging cases: (A) 300 g prostate, (B) big median lobe, (C) RSP post-TURP, (D) RSP in kidney transplant recipient, (E) salvage prostatectomy
(apex dissection), (F) bulky seminal vesicle sarcoma (CT scan on the left, beginning of the isolation on the right), and (G) prostatic sarcoma invading
the rectum (MRI on the left, urinary anastomosis on the right; the sigma anastomosed to the anus is visible on the posterior part of the image).
CT = computed tomography; MRI = magnetic resonance imaging; RSP = Retzius-sparing prostatectomy; TURP = transurethral resection of the prostate.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 6 8 6 – 6 8 8
687
















