
translated into a number needed to treat (NNT) to prevent a
recurrence at 10-yr follow-up of 5. However, no differences
were observed in the rate of metastasis-free survival and
cancer-specific mortality. The Southwest Oncology Group
(SWOG) 8794 trial included 450 patients with pT3N0 PCa
randomized to RT within 16 wk of surgery or initial
observation
[8]. At a median follow-up of 152 mo, the
10-year metastasis-free and overall survival rates were
significantly lower for patients treated with immediate RT
compared with observation (71% vs 61% and 74% vs 66%,
respectively). This translated into a NNT to prevent the
development of metastases in one case of 10. Similarly,
13 patients needed to be treated with immediate RT to
prevent one death. Although the results of these two trials
advocate aRT, approximately one-third of men in the
immediate RT group received RT in a salvage setting due
to detectable PSA levels immediately after surgery. These
individuals have worse metastases-free and overall survival
rates compared with their counterparts with complete
biochemical response
[84] .This issue was partially over-
come by the intention-to-treat analysis of the ARO 96–02
trial, which focused exclusively on patients with a PSA
<
0.5 ng/ml after RP
[7] .Overall, 307 men with pT3N0
disease at RP were randomized to aRT or observation. At a
median follow-up of 110 mo, individuals in the aRT group
had a 20% higher probability of being free from progression
compared with those in the observation arm (NNT: 5).
These findings support the role of immediate postoperative
RT in improving BCR-free survival in men with aggressive
disease characteristics, where approximately five patients
would need to receive immediate RT to prevent one
recurrence at 10-yr follow-up. Although only one study
demonstrated an effect of immediate RT after surgery on
stronger oncologic endpoints at long-term follow-up
[8], a
meta-analysis of these prospective randomized trials
demonstrated improved overall survival and reduced risk
of metastases
[85] .Differences in selection criteria, a lack of
systematic pathological quality assurance, heterogeneity in
radiation technique and dose, as well as the effectiveness of
salvage treatment are among the commonly proposed
explanations for the discrepancies between these studies
[6–8,86] .3.5.
How can we identify patients who would benefit from aRT?
Up to 40% of patients eligible for immediate RT according to
the inclusion criteria of randomized trials would not
experience BCR at 10-yr follow-up and may not thus
require additional cancer treatments
[6,7]. In a subset of
these individuals, the administration of aRT might repre-
sent
overtreatment
and be associated with patient inconve-
nience, expense, and a risk of short- and long-term side
effects ranging from 15% to 35% and 2% to 8%, respectively
[6–8,85,87,88]. Efforts have been made to improve our
ability to identify patients who would benefit from aRT and
thereby reduce the risk of overtreatment. In the subset
analyses of their randomized controlled trial, Thompson
et al
[8]demonstrated that the benefit of aRT in terms of
cancer-specific survival was greater in patients with higher-
grade disease. When considering 552 patients with
available pathologic review data included in the EORTC
trial 22911, the presence of positive surgical margins
represented the strongest predictor of BCR-free survival
after aRT
[34] .Therefore, aRT should be considered
particularly in men with positive margins at RP. Of note,
positive margins were an important predictor of recurrence
after pathologic review also in the ARO 96-02 trial
[37]. Abdollah et al
[31]evaluated a cohort of more than
1000 patients treated with RP aRT and suggested a benefit
[(Fig._2)TD$FIG]
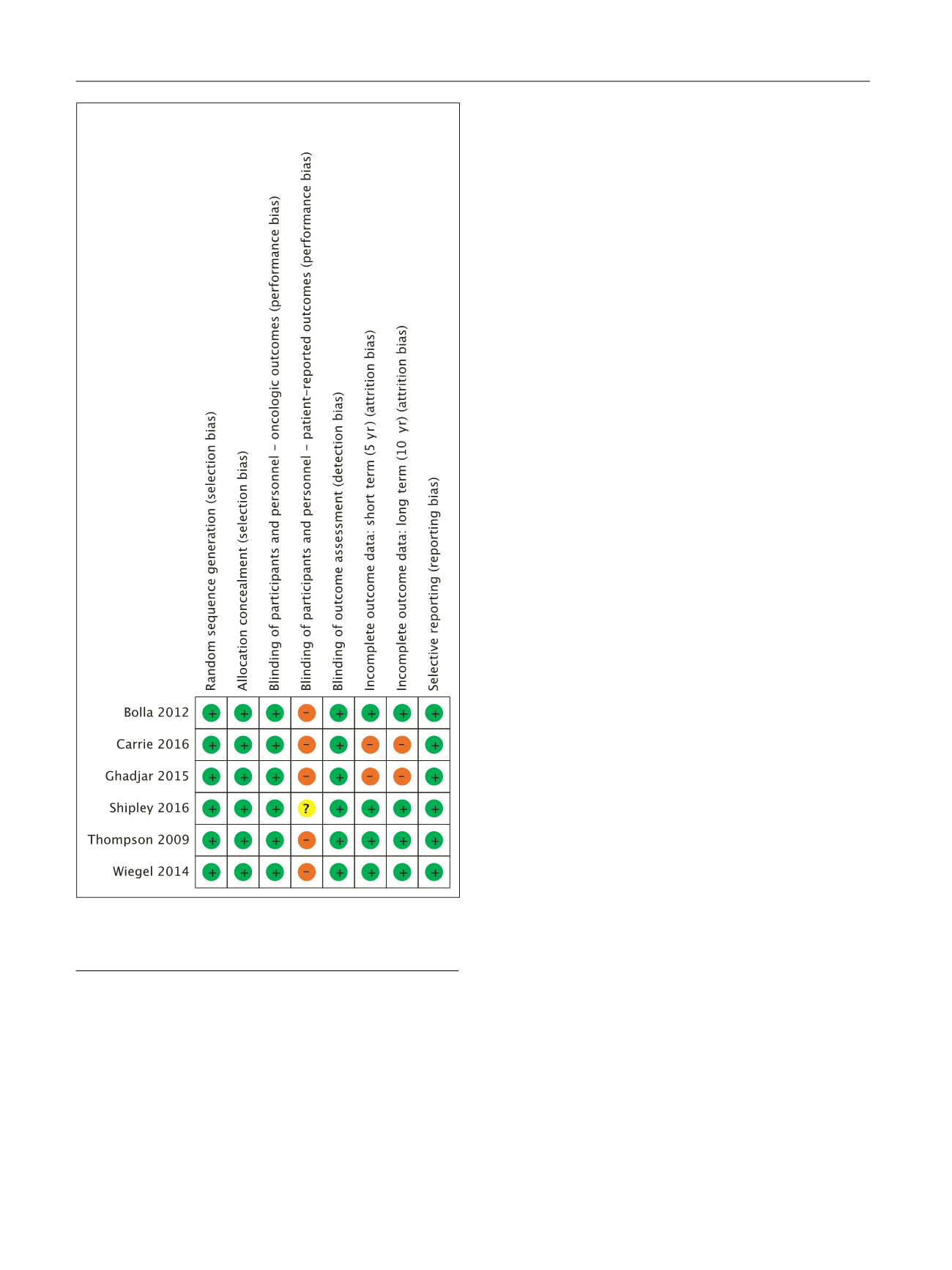
Fig. 2 – Risk of bias for randomized controlled trials included in the
systematic review (
n
= 6). Green indicates low risk, red indicates high
risk, and yellow indicates unclear.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 6 8 9 – 7 0 9
692
















