
biases. Moreover, the effect of confounders such as
pretreatment PSA, pathologic stage, and Gleason score could
not be excluded. Case series were at a high risk of bias
regarding the selection of consecutive patients and incom-
plete outcome data (attrition bias). Supplementary
Figure 1depicts the funnel plot that was generated to assess the
presence of publication bias in studies comparing the
progression-free survival of aRT versus sRT (
n
= 4).
3.3.
Rationale for postoperative RT in men with aggressive PCa
Historically, approximately 30% of PCa patients treated with
RP harbor extracapsular extension, seminal vesicle inva-
sion, high-grade disease, or lymph node invasion at final
pathology. With the decline of PSA screening and the
popularity of active surveillance, an increase in the
proportion of patients with more advanced disease among
those treated with RP has been observed
[31,75,76] .These
individuals are, in turn, at increased risk of recurrence after
surgery
[77]. Due to local disease aggressiveness, RP alone
may not be curative as it does not completely eliminate the
local tumor. The persistence of microscopic and advanced
disease increases the risk of recurrence and up to 50% of
men with post-RP BCR evaluated with molecular imaging
have pathologic uptake in the prostatic fossa or the pelvis
[5,78–81]. A multimodal approach aimed at maximizing
local regional control that includes postoperative RT might
reduce the risk of biochemical and clinical recurrence,
ultimately improving survival. This hypothesis inspired the
design of prospective randomized trials aimed at assessing
the role of postoperative RT in men with more aggressive
disease characteristics.
3.4.
Prospective randomized trials evaluating the role of aRT
aRT is defined as the administration of RT after surgery to
patients with aggressive disease characteristics in the
absence of signs of recurrence
[82] .Three randomized
trials addressing the role of postoperative RT have been
completed
( Table 1). The largest investigation is repre-
sented by the European Organization for Research and
Treatment of Cancer (EORTC) trial 22911, which random-
ized 1005 patients with pT2R1 or pT3N0 PCa to postopera-
tive RT within 16 wk from surgery versus initial
observation. After a median follow-up of 5 yr, aRT
significantly improved BCR and metastasis-free survival
[83]. At a median follow-up of 127 mo, immediate RT after
surgery reduced the risk of BCR
[6] .In particular, the 10-yr
BCR-free survival rates were 60.6 versus 41.1% for patients
treated with aRT or initial observation respectively. This
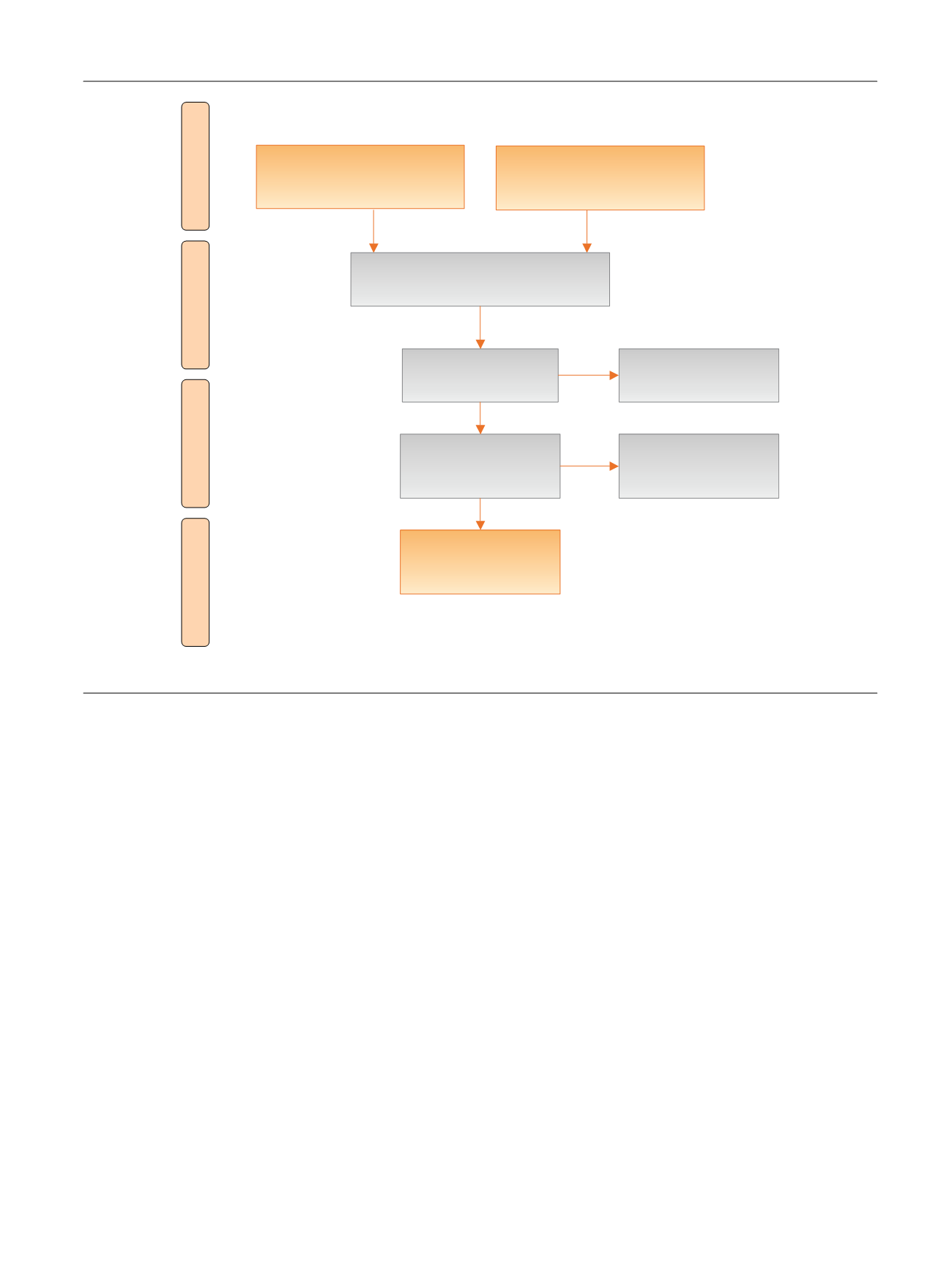
[(Fig._1)TD$FIG]
Records identified through
database searching
(
n
= 834)
Screening
Included
Eligibility
Identification
Additional records identified
through other sources
(
n
= 6)
Records after duplicates removed
(
n
= 352)
Records screened
(
n
= 352)
Records excluded
(
n
= 266)
Full-text articles
assessed for eligibility
(
n
= 86)
Full-text articles
excluded
(
n
= 16)
Studies included in
qualitative synthesis
(
n
= 70)
Fig. 1 – Preferred Reporting Items for Systematic Reviews flowchart.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 6 8 9 – 7 0 9
691
















