
1.51, 95% CI 1.03–2.21,
p
= 0.04; 0 pads/d OR 1.94, 95% CI
1.26–2.99,
p
= 0.003); interaction tests of approach with age
and nerve-sparing status were not significant. Patient age
and surgical approach were the strongest predictors of
urinary continence recovery in adequacy analyses (Supple-
mentary Tables 1 and 2). LOESS curves did not show a change
in 24-h pad weights (at any time point) with increasing case
experience (Supplementary Fig. 1–4).
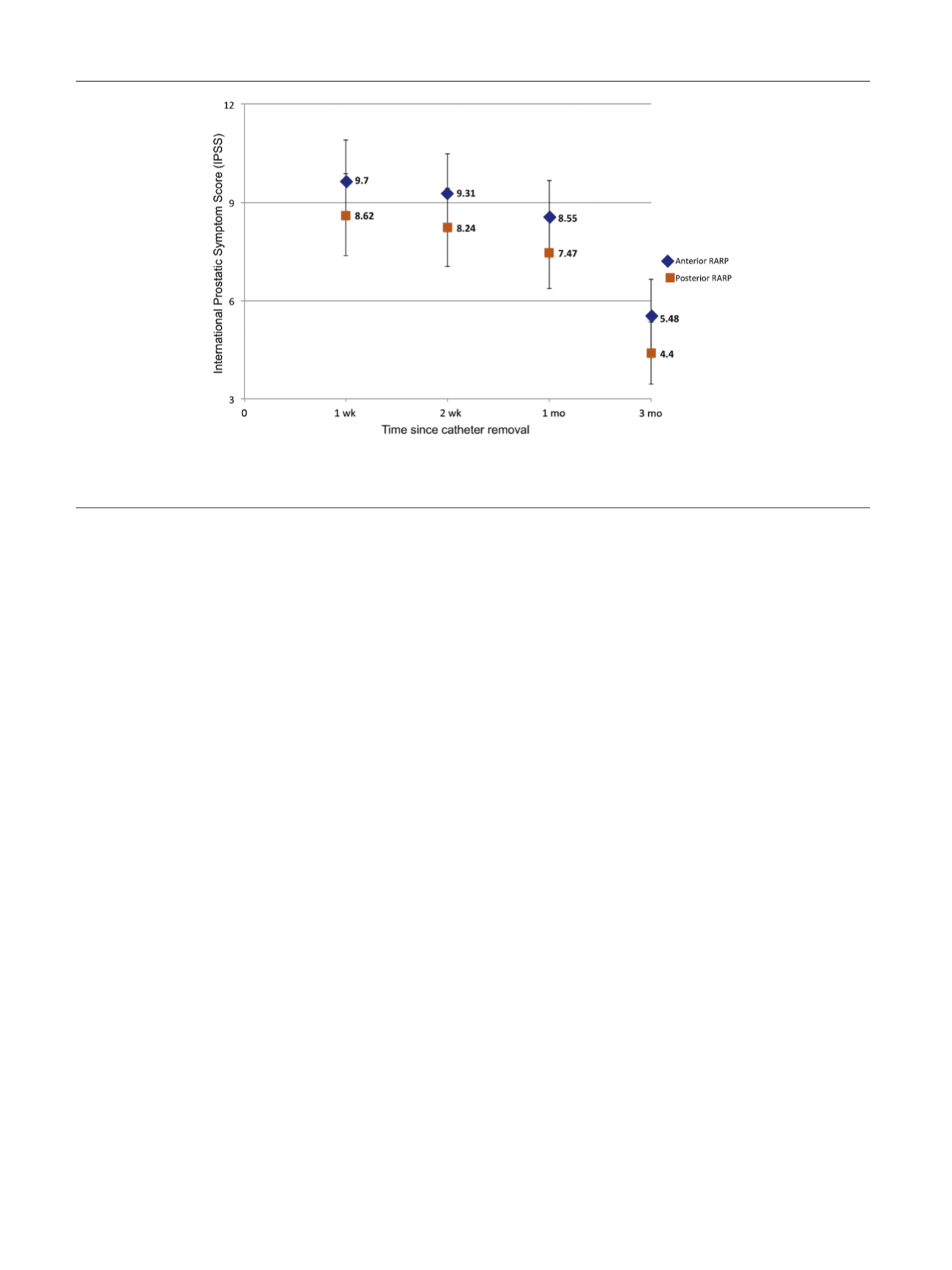
On GEE analysis, the mean IPSS urinary function scores
were not significantly different between the two cohorts at
any measured time point following catheter removal
( Fig. 4 ). Mean urinary bother scores were significantly
lower in the posterior versus anterior RARP arm
[24_TD$DIFF]
at
[25_TD$DIFF]
1 wk,
2 wk and 1 month
( Fig. 5). The surgical approach was
independently associated with urinary bother but not
urinary function scores (Supplementary Tables 3 and 4).
3.4.
Secondary outcomes: perioperative complications and
margin rates
There were no intraoperative complications in either arm.
Incidence of any postoperative complication was 12% versus
18% in anterior versus posterior arms (
p
= 0.9; Supplemen-
tary Table 5), including lymphoceles requiring percutaneous
drainage (
n
= 4 in anterior and
n
= 5 in posterior). Overall
PSM rates were 13% for the anterior versus 25% for the
posterior approach (
p
= 0.1); the corresponding rates of
nonfocal ( 2 mm) margins were 8% and 12%, respectively
(
p
= 0.2). The probability of BCRFS was 0.91 (95% CI
[26_TD$DIFF]
0.83–
[27_TD$DIFF]
1.0)
for anterior versus 0.91 (
[28_TD$DIFF]
0.83–
[29_TD$DIFF]
0.99) for posterior RARP
(
p
= 0.5), with a hazard ratio of 0.78 (0.21–2.91).
4.
Discussion
Within the last decade, a number of technical modifications
have been suggested to improve urinary continence in
patients undergoing RARP
[8,22,23] .Schuessler et al
[24]were the first to describe the Retzius-sparing approach in a
series of nine patients undergoing laparoscopic RP. Addi-
tionally, large-scale studies by Prabhu et al
[6], Donovan
et al
[7], and Sanda et al
[3]have already shown that the
highest rates of urinary incontinence are seen 2–6 mo after
surgery, which improve thereafter. With these consider-
ations in mind, we designed an RCT to assess the impact of
the posterior approach on improving short-term ( 3 mo)
urinary continence recovery in comparison with our
standard anterior RARP. This, to our knowledge, represents
the first level 1 evidence for the Retzius-sparing approach.
We noted that 71% of patients undergoing posterior
RARP were continent 1 wk after catheter removal (com-
pared with 48% with anterior approach), which increased to
83% (vs 67%) and 95% (vs 86%) at 1 and 3 mo, respectively.
Surgical approach (posterior vs anterior RARP), along with
patient age, was one of the strongest predictors of urinary
continence recovery. While urinary continence in anterior
approach patients was comparable with what we have
reported previously
[25], patients undergoing posterior
RARP demonstrated one of the highest observed rates of
urinary continence in a level 1 study
[8] ,with a median time
to urinary continence recovery of 2 d postcatheter removal.
As such, our findings corroborate those of Galfano et al
[10]and Lim et al
[26]. However, these studies comprised highly
selected patients with no concurrent matched controls, and
were limited by subjective assessment of the number of
pads. Additionally, few prior reports quantified the effect of
the RP approach on continence outcomes using pad weights
[15,27]. In our study, patients in the posterior RARP arm
consistently showed a median 24-h pad weight of 0 g at all
study time points, while 24-h pad weights in the control
arm decreased from 25 g at 1 wk to 5 and 0 g at 1 and 3 mo,
respectively
[5_TD$DIFF]
. While our study was not designed to provide a
mechanistic explanation for earlier continence recovery
[(Fig._4)TD$FIG]
Fig. 4 – Mean IPSS urinary function (UF) scores at 1
[6_TD$DIFF]
week
[7_TD$DIFF]
(wk
[8_TD$DIFF]
), 2 wk, 1
[9_TD$DIFF]
month
[10_TD$DIFF]
(mo
[11_TD$DIFF]
), and 3 mo (following catheter removal) in patients undergoing
anterior versus posterior robot-assisted radical prostatectomy (RARP). Numbers along
Y
-axis represent estimates derived from generalized estimating
equations. Error bars represent 95% confidence intervals. IPSS = International
[12_TD$DIFF]
Prostate Symptom Score.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 6 7 7 – 6 8 5
682
















