
median lobes, post-transurethral resection of the prostate
(post-TURP), kidney transplant recipients, salvage prosta-
tectomies, seminal vesicle or prostatic sarcomas invading
the rectum
( Fig. 2 ).
This trial represents a further step toward RSP being
accepted by the scientific community as a standard
approach for prostate-cancer surgery. In fact, according to
the IDEAL protocol of surgical development appraisal
[6],
the Retzius-sparing approach successfully went beyond
the
innovation stage
following our 2010 publication
[7];
the
developmental stage
was reached in 2011 with the
evaluation of the first 20 operated patients, which
confirmed the excellent results regarding continence
[8].
In 2013, the first 200 prospective case series allowed us to
reach the
exploration stage
[4]. The next stage of the
protocol—
assessment
—aims to compare the results of inno-
vative and standard treatment. Together with the previously
published nonrandomizedmatched pair analysis by Lim et al
[9] ,the paper by Dalela et al does just this. Only the lack of
long-term results fails to make RSP a new standard in radical
prostatectomy. However, that is about to end.
Future papers on this topic need to focus mainly on
oncological results. Our first cases were challenged by a
high positive surgical margin (PSM) rate. We justified this
by the fact that it involved a series of patients in whom
technical refinement was taking place; the next patients
reported by our group and the consequent published series
confirmed our impressions, lowering the PSM rate to that
reported in the literature
[10] .The current paper did
not focus on the PSM rate, but reports a nonsignificant
trend (overall, nonstratified per T stage 13% vs 25%,
p
= 0.1—mostly focal) between the two groups. In this case
too, we are comparing two techniques with significant
differences in the background experience of the surgeon
(60 vs thousands of cases). Moreover, there is no reason to
imagine different oncological results: in the era of multi-
parametric magnetic resonance imaging, a millimetric
surgical plan can be preoperatively defined to avoid PSM,
whatever approach might be used.
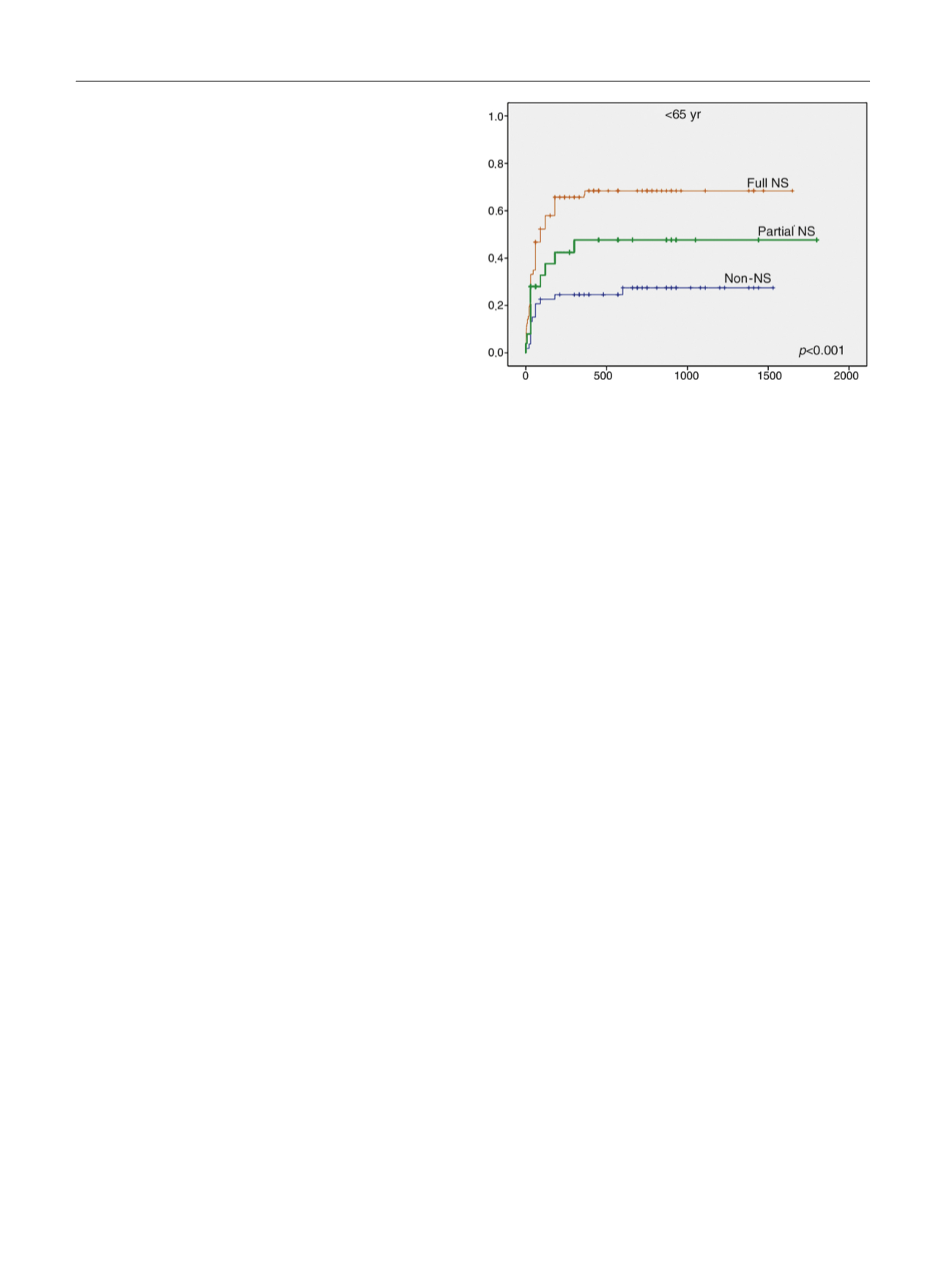
The focus should then pass to sexual function. Data from
our series
( Fig. 3) show that potency recovery appears to be
not palpably different from the published series, with
roughly 70% of patients under 65 yr recovering erection 1 yr
after full nerve-sparing surgery. On the contrary, it seems
that patients undergoing non–nerve-sparing surgery have
an unexpectedly high 1-yr potency rate (21%). A role played
by the vascular and neuronal network situated in the
anterior compartment up to the Santorini plexus might be
hypothesized, but further research is clearly needed.
In conclusion, a huge number of surgical innovations
have passed like meteors in the urological sky, disappearing
long before an RCT showed that they were no better than
the standard technique. We really thank professor Menon
and his team for their research because we are aware that it
will facilitate the permeation of RSP, transforming it from a
possible passing meteor into a new shining star.
Conflicts of interest:
The authors declare that they have no pending
conflicts of interest.
References
[1]
Dalela D, Jeong W, Prasad MA, et al. A pragmatic randomized controlled trial examining the impact of the Retzius-sparing ap- proach on early urinary continence recovery after robot-assisted radical prostatectomy. Eur Urol 2017;72:677–85.[2]
Menon M, Shrivastava A, Bhandari M, Satyanarayana R, Siva S, Agarwal PK. Vattikuti Institute prostatectomy: technical modifica- tions in 2009. Eur Urol 2009;56:89–96.[3] Abdollah F, Dalela D, Sood A, et al. Functional outcomes of clinically
high-risk prostate cancer patients treated with robot-assisted radi-
cal prostatectomy: a multi-institutional analysis. Prostate Cancer
Prostatic Dis. In press.
http://dx.doi.org/10.1038/pcan.2017.26 .[4]
Galfano A, Di Trapani D, Sozzi F, et al. Beyond the learning curve of the Retzius-sparing approach for robot-assisted laparoscopic radi- cal prostatectomy: oncologic and functional results of the first 200 patients with 1 year of follow-up. Eur Urol 2013;64:974–80.[5]
Ficarra V, Novara G, Rosen RC, et al. Systematic review and meta- analysis of studies reporting urinary continence recovery after robot-assisted radical prostatectomy. Eur Urol 2012;62:405–17.[6]
McCulloch P, Altman DG, Campbell WB, et al. No surgical innovation without evaluation: the IDEAL recommendations. Lancet 2009;374: 1105–12.[7]
Galfano A, Ascione A, Grimaldi S, Petralia G, Strada E, Bocciardi AM. A new anatomic approach for robot-assisted laparoscopic prosta- tectomy: a feasibility study for completely intrafascial surgery. Eur Urol 2010;58:457–61.[8]
Galfano A, Ascione A, Prestini G, Grimaldi S, Bocciardi AM. 348 A new Retzius-sparing anatomic approach for RALP. Preliminary results from the first 20 cases of a totally intrafascial technique. Eur Urol Suppl 2011;10:126–7.[9]
Lim SK, Kim KH, Shin TY, et al. Retzius-sparing robot-assisted laparoscopic radical prostatectomy: combining the best of retro- pubic and perineal approaches. BJU Int 2014;114:236–44.[10]
Novara G, Ficarra V, Mocellin S, et al. Systematic review and meta- analysis of studies reporting oncologic outcome after robot- assisted radical prostatectomy. Eur Urol 2012;62:382–404.
[(Fig._3)TD$FIG]
Fig. 3 – Erectile function recovery in patients younger than 65 yr.
NS = nerve sparing.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 6 8 6 – 6 8 8
688
















