
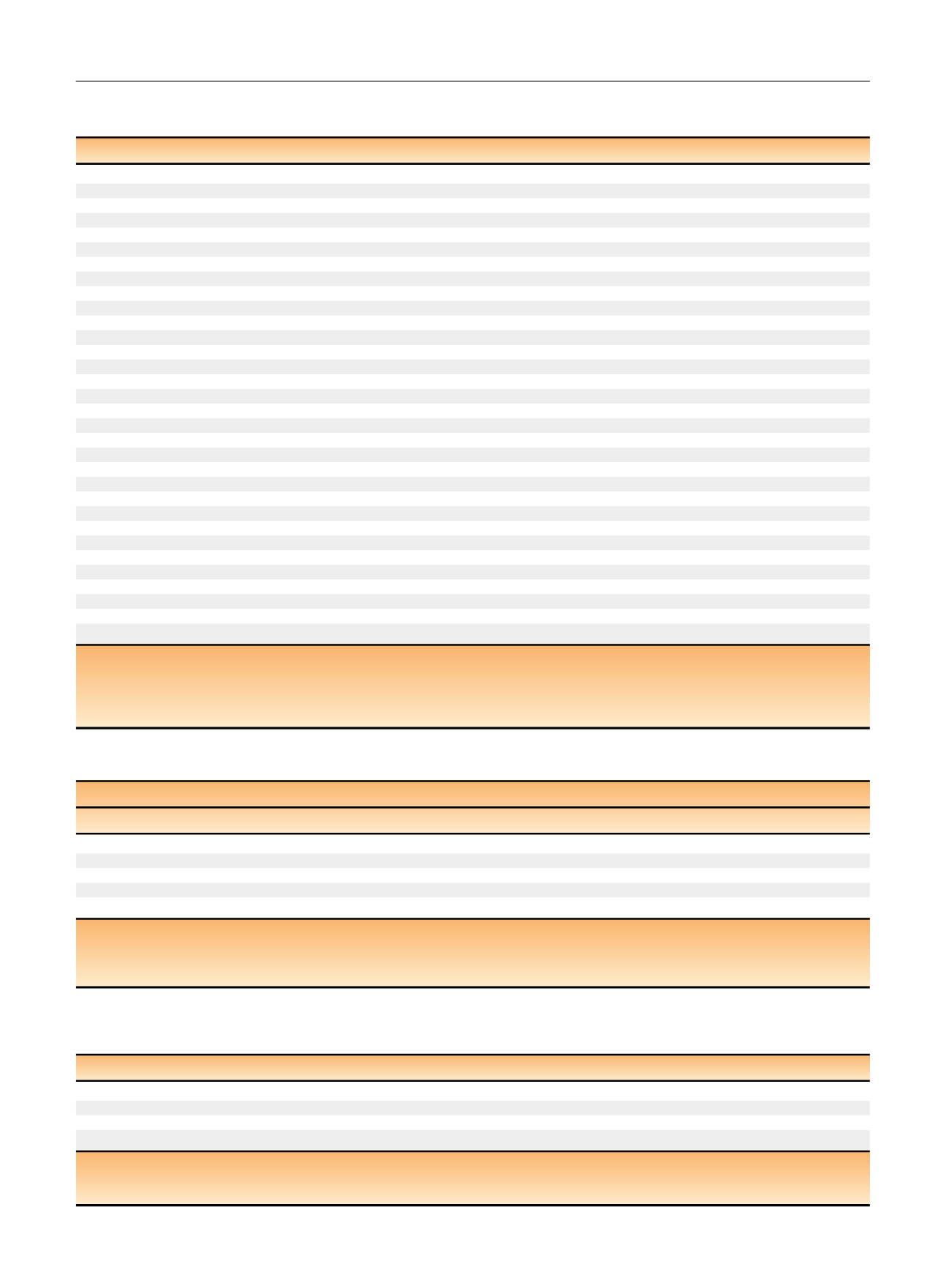
Table 1 – Relevant demographic and clinical variables for patients undergoing anterior or posterior approach robot-assisted radical
prostatectomy (RARP) by a single surgeon at the Vattikuti Urology Institute (January 2015–April 2016)
Characteristic
Anterior RARP (
n
= 60)
Posterior RARP (
n
= 60)
Age (yr), median (IQR)
61.5 (56–67)
61.0 (55–67)
BMI (kg/m
2
), median (IQR)
28.0 (26.4–30.9)
27.9 (26.1–30.6)
ASA score, median (IQR)
2 (2–3)
2 (2–3)
Diabetes mellitus (type 2),
n
(%)
11 (18)
5 (8)
Smoking status,
n
(%)
Never smoker
33 (55)
38 (63)
[16_TD$DIFF]
Former smoker
17 (28)
16 (27)
[17_TD$DIFF]
Current smoker
7 (12)
4 (6.7)
[18_TD$DIFF]
Unknown
3 (5)
2 (3.3)
[3_TD$DIFF]
Preoperative IPSS UF score, median (IQR)
6.5 (3–13)
7 (3–12)
Preoperative UF-related bother score, median (IQR)
2 (0–3)
2 (1–2)
Preoperative SHIM score, median (IQR)
20 (8–25)
20 (14–24)
Preoperative PSA (ng/ml), median (IQR)
5.4 (3.7–7.3)
5.7 (4.7–7.4)
Clinical stage,
n
(%)
cT1c
46 (78)
40 (67)
cT2a–T2b
12 (20)
19 (32)
cT2c
1 (1.7)
1 (1.7)
Biopsy Gleason,
n
(%)
3 + 3
20 (33)
18 (30)
3 + 4
26 (43)
34 (57)
4 + 3
14 (23)
8 (13)
NCCN risk group,
n
(%)
Low
15 (25)
14 (23)
Intermediate
45 (75)
46 (77)
Prior abdominal surgery
a[15_TD$DIFF]
,n
(%)
29 (48)
24 (40)
Nerve sparing,
n
(%)
Veil (bilateral)
39 (65)
37 (62)
Standard (uni/bilateral)
21 (35)
23 (38)
PLND,
n
(%)
None
4 (6.7)
5 (8.3)
Limited/standard
53 (88)
47 (78)
Extended
3 (5.0)
8 (13)
IQR = interquartile range; BMI = body mass index; ASA = American Society of Anesthesiologists; IPSS = International
[12_TD$DIFF]
Prostate Symptom Score; UF = urinary
function; SHIM = Sexual Health Inventory for Men; PSA = prostate-specific antigen; NCCN = National Comprehensive Cancer Network; PLND = pelvic lymph
node dissection.
Percentages may not add up to 100% due to rounding.
a
Includes prior appendectomy, inguinal/umbilical hernia repair, diverticulectomy, laparotomy, small bowel resection, or surgery of the descending colon.
Table 2 – Urinary continence outcomes 1
[6_TD$DIFF]
week
[7_TD$DIFF]
(wk
[19_TD$DIFF]
) after catheter removal for 119 patients undergoing anterior (
n
= 60) or posterior approach
(
n
= 59) robot-assisted radical prostatectomy (RARP) by a single surgical team at the Vattikuti Urology Institute (January 2015–April 2016)
Intent-to-treat analysis
Outcome
Anterior RARP (
n
= 60) Posterior RARP (
n
= 59) Difference in estimates (95% CI)
p
value
Continent (0 pads/one security pad per day),
n
(%)
29 (48)
42 (71)
23 (5.2–39) %
0.01
aContinent (0 pads/d),
n
(%)
9 (15)
25 (42)
27 (11–42)%
0.001
a24-h pad weight (g), median (IQR)
Overall
25 (3–133)
5 (0–25)
20 (6–34)
0.002
bPatients wearing security pad
10 (4–29)
8 (5–25)
2 (0–14)
0.7
bCI = confidence interval; IQR = interquartile range.
CI for difference in proportions calculated with continuity correction.
a
p
value calculated using Pearson chi-square test.
b
p
value calculated using Mann–Whitney
U
test.
Table 3 – Distribution of median 24-h pad weights 1
[6_TD$DIFF]
week
[7_TD$DIFF]
(wk
[8_TD$DIFF]
), 2 wk, 1
[9_TD$DIFF]
month
[10_TD$DIFF]
(mo
[11_TD$DIFF]
), and 3 mo after catheter removal in patients undergoing
anterior versus posterior robot-assisted radical prostatectomy (RARP) by a single surgical team at the Vattikuti Urology Institute
[21_TD$DIFF]
(January
2015–April 2016)
Time since catheter removal
Anterior RARP
Posterior RARP
Difference in medians (95% CI)
a[20_TD$DIFF]
p
value
b1 wk
25 (4–133)
5 (0–27)
20 (6–34)
0.002
2 wk
12 (0–82)
0 (0–18)
12 (2–22)
0.004
1 mo
5 (0–72)
0 (0–7)
5 (–4–14)
0.001
3 mo
0 (0–7)
0 (0–0)
0 (0–0)
0.1
CI = confidence interval.
a
95% CIs for difference in medians calculated using the Bonett and Price method
[30] .b
p
value calculated using Mann–Whitney
U
test.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 6 7 7 – 6 8 5
680
















