
incontinent patients measuring 24-h pad weights
[16]. Procedure-
specific postoperative complications (reported using Donat criteria
[17])
were captured comprehensively using multiple sources (as described
earlier
[18]). Oncological outcomes were positive surgical margins
(PSMs; focal [
<
2 mm] and nonfocal [ 2 mm]) and probability of
biochemical recurrence-free survival (BCRFS) at 1-yr follow-up.
Data were collected by an independent database manager and stored
in a password-protected Microsoft Excel file. The operating surgeon,
surgical team, and supporting personnel involved in postoperative care
did not have access to the data files.
2.2.
Statistical analyses
Nonparametric Mann–Whitney tests and Pearson chi-square/Fisher’s
exact tests were used to detect significant differences in continuous and
categorical variables, respectively, between the two study arms. Control of
multiple comparisons in the test comparing proportions of patients with
different levels of urinary incontinence at different time points was
achieved using Bonferroni correction. Urinary continence recovery rates
were modeled using the Kaplan–Meier method, and its association with
surgical approach was tested using a Cox proportional hazards model,
adjusted for age, American Society of Anesthesiologists (ASA) score, and
nerve sparing status (veil vs standard
[19]). Additionally, we performed a
priori specified ‘‘adequacy’’ analysis
[20]to identify the most important
factors associated with continence recovery (Supplementary material).
Linear generalized estimating equations (GEEs) were used to account for
repeated measures when assessing for statistically significant changes in
urinary function and urinary bother scores between the two arms
[21]. Separate GEE models were used to identify the independent effect of
treatment armon urinary function and urinary bother, after controlling for
the effect of age, ASA score, and nerve sparing status (Supplementary
material).
Missing data were not imputed, and an intent-to-treat analysis was
performed. We also performed an a priori specified per-protocol analysis
of our primary outcome. Statistical analyses were performed using SPSS
version 21 (IBM Corp., Armonk, NY, USA) SAS version 9.4 (SAS Institute,
Inc., Cary, NC, USA) by an independent, dedicated biostatistician
uninvolved in the study and blinded to treatment assignment. We
planned an interim analysis using Pocock two-sided symmetric bound-
aries when 50% of the data were obtained. These define an alpha of 0.03 in
the interim analysis and 0.02 at the end when all data are available. A
p
value of
<
0.05 was considered significant for the secondary outcomes.
3.
Results
3.1.
Baseline demographics
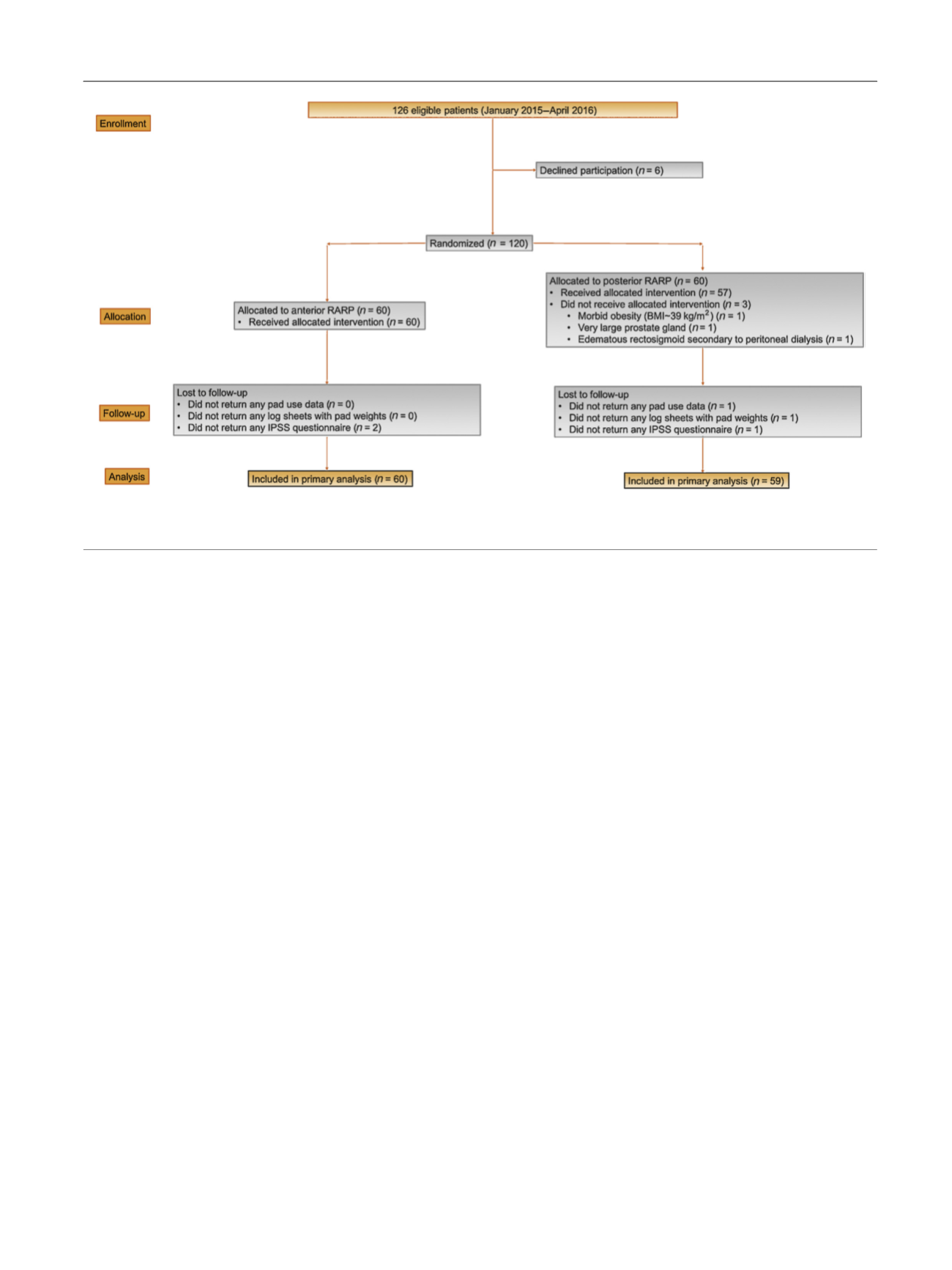
A total of 120 consecutive, eligible, and consenting patients
were randomized to receive either an anterior (
n
= 60) or a
posterior approach (
n
= 60; of these, three patients were
converted to the anterior approach). Notably, 75% and 77% of
patients in the anterior and posterior arms, respectively,
harbored NCCN intermediate-risk disease
( Table 1). Thirty-
nine (65%) patients in the anterior and 37/60 (62%) in the
posterior RARP arm underwent bilateral veil nerve sparing
(
p
= 0.9).
3.2.
Primary outcome: urinary continence at 1 wk after
catheter removal
In the intent-to-treat analysis
( Table 2 ), 71% versus 48%
patients were continent (0 pads/one security pad per day)
1 wk after catheter removal in the posterior versus anterior
group (
p
= 0.01); corresponding pad-free rates were 42%
and 15%, respectively (
p
= 0.001). The median (interquar-
tile range) 24-h pad weights were 5 (0–25) g in the
posterior and 25 (3–133) g in the anterior RARP arms
(
p
= 0.001) overall. Similar results were noted in
[(Fig._1)TD$FIG]
Fig. 1 – CONSORT diagram explaining the flow of participants through the trial. RARP = robot-assisted radical prostatectomy; IPSS = International
Prostatic Symptom Score; BMI = body mass index.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 6 7 7 – 6 8 5
679
















