
1.
Introduction
Up to 70% of patients with non–muscle-invasive bladder
cancer (NMIBC) have tumour recurrence, and about 10–15%
progress to muscle-invasive disease
[1] .Accurate prediction
of tumour recurrence and progression is important to
determine appropriate therapy and follow-up. Tumour
grade is an important predictor of tumour prognosis
[2] .However, histopathological classifications are known
to be limited by inter- and intraobserver variability, which
may have profound prognostic implications
[3].
Current European Association of Urology (EAU) recom-
mendations for grading of NMIBC indicate that both the
1973 and the 2004/2016 World Health Organization (WHO)
classification should be used
[4]. The 1973 classification
distinguishes three different grades and evaluates micro-
scopic features related to the degree of cellular atypia,
necrosis, and mitotic activity. Grade 1 (G1) carcinomas
(well-differentiated) are defined as showing only mild
degrees of cytological atypia and infrequent mitotic figures.
Grade 3 (G3) carcinomas (poorly differentiated) are defined
as showing marked nuclear pleomorphism, loss of matura-
tion from the base to the surface, and mitotic activity. Grade
2 (G2) carcinomas (moderately differentiated) comprise all
tumours between these extremes
[5]. The lack of clarity
between the three grades may adversely affect prognostic
prediction due to high intra- and interobserver variability.
Furthermore, there is a tendency to classify the majority of
tumours in the middle group (G2)
[6].
In an attempt to reduce variability and increase
reproducibility, a new grading system based on more
detailed histological criteria has been promoted since
1998 by the International Society of Urological Pathology
(ISUP) and was subsequently adopted by the WHO in
2004. The main aim was to standardise the classification
and grading of urothelial neoplasms, creating a uniform
terminology for use by pathologists and urologists
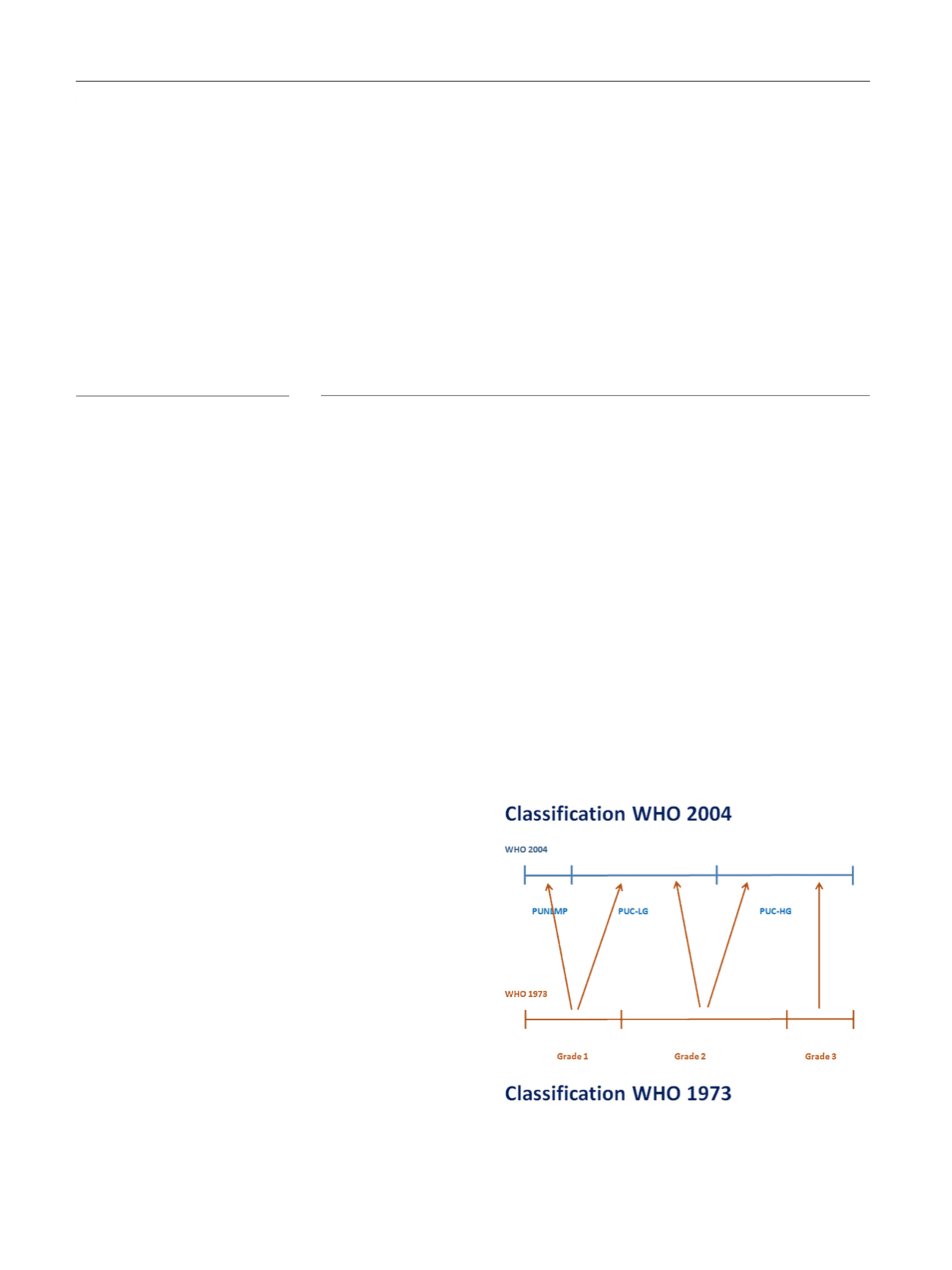
[7,8]. Un-
der the 2004 system, some G1 lesions are classified as
papillary urothelial neoplasms with low malignant poten-
tial (PUNLMPs) and others are classified as low grade (LG);
G2 lesions are classified as LG or high-grade (HG) urothelial
carcinomas; G3 lesions as HG urothelial carcinomas
( Fig. 1). Recently, an update of the 2004 WHO grading
classification was published without substantial changes,
so the 2004 WHO classification is now known as 2016 WHO
classification
[9].
By eliminating the heterogeneous moderately differen-
tiated (G2) category of the 1973 system, the 2004/2016
classification was expected to provide a more reproducible
stratification of patients with differing prognoses and well-
defined recommendations for treatment and follow-up.
However, several studies have shown considerable inter-
observer variability and its anticipated superior prognostic
value is still a matter of debate
[6,10].
This systematic review compares the prognostic perfor-
mance and reproducibility of the 1973WHO and 1998 ISUP/
2004 WHO/2016 WHO grading systems for NMIBC.
Evidence synthesis:
Of 3593 articles identified, 20 were included in the prognostic review;
three were eligible for the reproducibility review. Increasing tumour grade in both
classifications was associated with higher disease progression and recurrence rates. Pro-
gression rates in grade 1 patients were similar to those in low-grade patients; progression
rates in grade 3 patients were higher than those in high-grade patients. Survival data were
limited. Reproducibility of the 2004/2016 system was marginally better than that of the
1973 system. Two studies on repeatability showed conflicting results. Most studies had a
moderate to high risk of bias.
Conclusions:
Current grading classifications in NMIBC are suboptimal. The 1973 system
identifies more aggressive tumours. Intra- and interobserver variability was slightly less in
the 2004/2016 classification. We could not confirm that the 2004/2016 classification
outperforms the 1973 classification in prediction of recurrence and progression.
Patient summary:
This article summarises the utility of two different grading systems for
non–muscle-invasive bladder cancer. Both systems predict progression and recurrence,
although pathologists vary in their reporting; suggestions for further improvements are
made.
#
2017 European Association of Urology. Published by Elsevier B.V. All rights reserved.
2004/2016 World Health
Organization classification
Prognosis
Recurrence
Progression
Repeatability
Reproducibility
[(Fig._1)TD$FIG]
Fig. 1 – Stratification of tumours according to grade in the 1973 and
2004 WHO classifications. PUNLMP = papillary urothelial neoplasm with
low malignant potential; PUC-LG = papillary urothelial carcinoma—low
grade; PUC-HG = papillary urothelial carcinoma—low grade;
WHO = World Health Organization.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 8 0 1 – 8 1 3
802
















