
conducting in-depth interviews with healthcare profes-
sionals involved in recruitment and patients approached
about the study, audio recording recruitment discussions,
analysing screening log data to understand patient pathways,
observing study meetings, and reviewing study documenta-
tion, with rapid analysis of findings and reporting to the CI
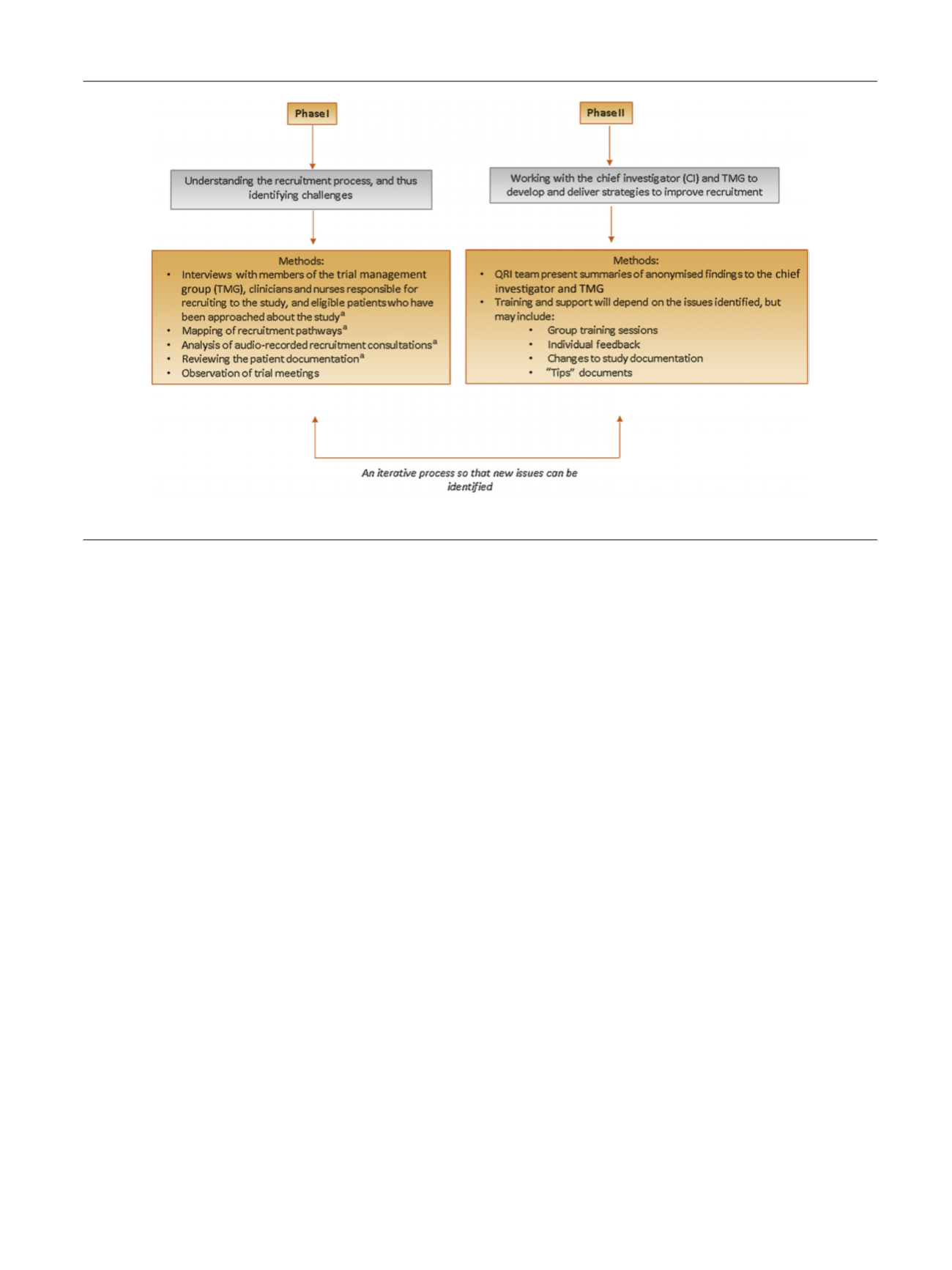
and trial management group (TMG). In phase 2, the QRI team
works collaboratively with the CI and TMG to implement
strategies to improve recruitment (see
Fig. 2)
[26] .To date,
these methods have been implemented in 25 RCTs. The QRI
has optimised methods that enable recruitment to be
completed in feasibility/pilot or main RCTs
[25,26, 31,52] .In other instances, the QRI has provided detailed
evidence to support a decision to cease recruitment
[32] .3.3.2.
Challenges of integrating qualitative research in RCTs
Whilst these methods produce important insights about
recruitment practices, the challenges of integrating quali-
tative research with RCTs has been well documented. For
instance, recruiters are often reluctant to provide audio
recordings of consultations
[24,26,38,44,50,52] .If the
qualitative research is integrated into an RCT where
recruitment is already ongoing, the process of obtaining
additional ethical approval can be lengthy
[26]. It has
therefore been suggested that qualitative work should be
integrated structurally and culturally into the RCT, ideally
before recruitment begins and at the feasibility stage, in
order to produce the greatest results
[50].
3.3.3.
Future directions for research
It is important to note that current interventions are limited
by the availability of only observational evidence of their
effectiveness, therefore limiting the ability to determine
causality between interventions and recruitment rates
[26]. A recent review has identified the need to develop
more robust designs to develop an evidence base on how
best to support recruiters
[59]. More robust studies are
needed to assess the effectiveness of training programmes,
although these will need to give careful consideration to
how ‘‘successful’’ interventions should be defined (ie,
completion of study or evidence to support closure) and
what the outcomes should be (ie, screening and eligibility
counts, recruitment rates, or changes in informed consent).
Furthermore, given that research has demonstrated that
patients can find RCT concepts confusing
[14–17] ,it is
important not to neglect the patient’s perspective of the
recruitment process, and to further develop methods to
facilitate joint decision making and ensure fully informed
consent.
4.
Conclusions
Many fundamental questions in the management of
patients in most specialities remain unanswered, and RCTs
are required to provide high-quality evidence to support
clinical decision making. Recruitment difficulties were
often attributed to logistical issues (such as a lack of time
for research activities) or patient-related factors (including
strong treatment preferences or disliking randomisation).
In 2012, Fletcher and colleagues
[18]highlighted the
potential of using qualitative research to understand
recruitment, and since this, qualitative studies have shed
further light on the challenges of recruiting patients
[24,26– 29,31–34,36–38,40,43,45,48,49,52–54]. Taken together,
these highlight how recruitment is a complex and fragile
process in which recruiters can experience emotional and
[(Fig._2)TD$FIG]
Fig. 2 – Overview of the QuinteT Recruitment Intervention.
a
Actions are mandatory.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 7 8 9 – 7 9 8
795
















