
treatment preferences for particular interventions
[23– 25,27,32,35,44,52,53] .Aside from recruiter influences,
patient preferences can be informed by a number of factors,
including information and advice from family and friends
[25]and the media
[25]. Mills and colleagues
[41]conducted an analysis of audio recordings of recruitment
appointments with 93 participants in a trial of localised
prostate cancer treatments. Patient preferences ranged
from hesitant opinions to well-formed intentions to receive
a particular treatment. These preferences frequently
changed after detailed discussion of treatments and trial
rationale with recruitment staff. However, several studies
have highlighted that recruiters can feel uncomfortable
exploring these further
[24,32,40,44,52]and are more likely
to accept patient preferences if they align with the
recruiter’s own views
[27,28].
3.2.7.
Identifying specific recruitment issues in RCTs
Whilst the challenges identified are commonly reported
across a range of RCTs, it is important to note that the degree
that these issues are present and the extent that they affect
recruitment will inevitably vary between RCTs. For in-
stance, whilst recruiters often struggle to feel comfortable
with the concept of uncertainty between trial arms, training
and support strategies can sometimes help overcome this so
that recruitment targets are met
[25]. In other instances, the
lack of recruiter equipoise has been so fundamental that the
RCT had to be closed
[32] .In addition to these common themes, each RCT will have
a set of unique issues that need to be resolved
[50] .Urologi-
cal RCTs often involve complicated pathways that can be
particularly lengthy, and include many different healthcare
professionals or multiple centres
[44] .The availability and
evidence base for treatment options outside of each RCT will
vary (particularly within fields such as urology, where there
are rapidly changing treatment options
[23]), which may
have implications for clinician equipoise. Some RCTs may
also have complex designs, making them even more
difficult to discuss with patients. For instance, recruiters
from one urological trial had to explain the need for
neoadjuvant chemotherapy, the timing of randomisation in
relation to the cycles of chemotherapy, and two extremely
different treatment arms (surgery to remove the cancer and
bladder, or a selective bladder preservation technique that
involved radiotherapy to destroy the cancer and preserve
the bladder except where the tumour persisted when
surgery was recommended)
[44].
3.3.
Part 2: what solutions are there to recruitment difficulties?
3.3.1.
Developing training programmes for those recruiting to trials
Taken together, the previous section has highlighted the
need for training and support for recruiters (both for generic
and RCT-specific issues). Only a relatively small number of
studies have used qualitative research to develop training
for those recruiting patients into RCTs
[24,26,31,32,38,44, 50,52] .One study developed a peer-review training
programme, whereby four research nurses from an
orthopaedic pilot study provided regular feedback on each
other’s recorded RCT consultations. All the nurses felt that
communication and recruitment abilities were improved,
and stated that they would want to repeat this process in
subsequent trials
[38].
The other interventions identified had originated from
the ProtecT study
[4_TD$DIFF]
, whereby a complex intervention was
developed to improve rates of randomisation and informed
consent
[25].
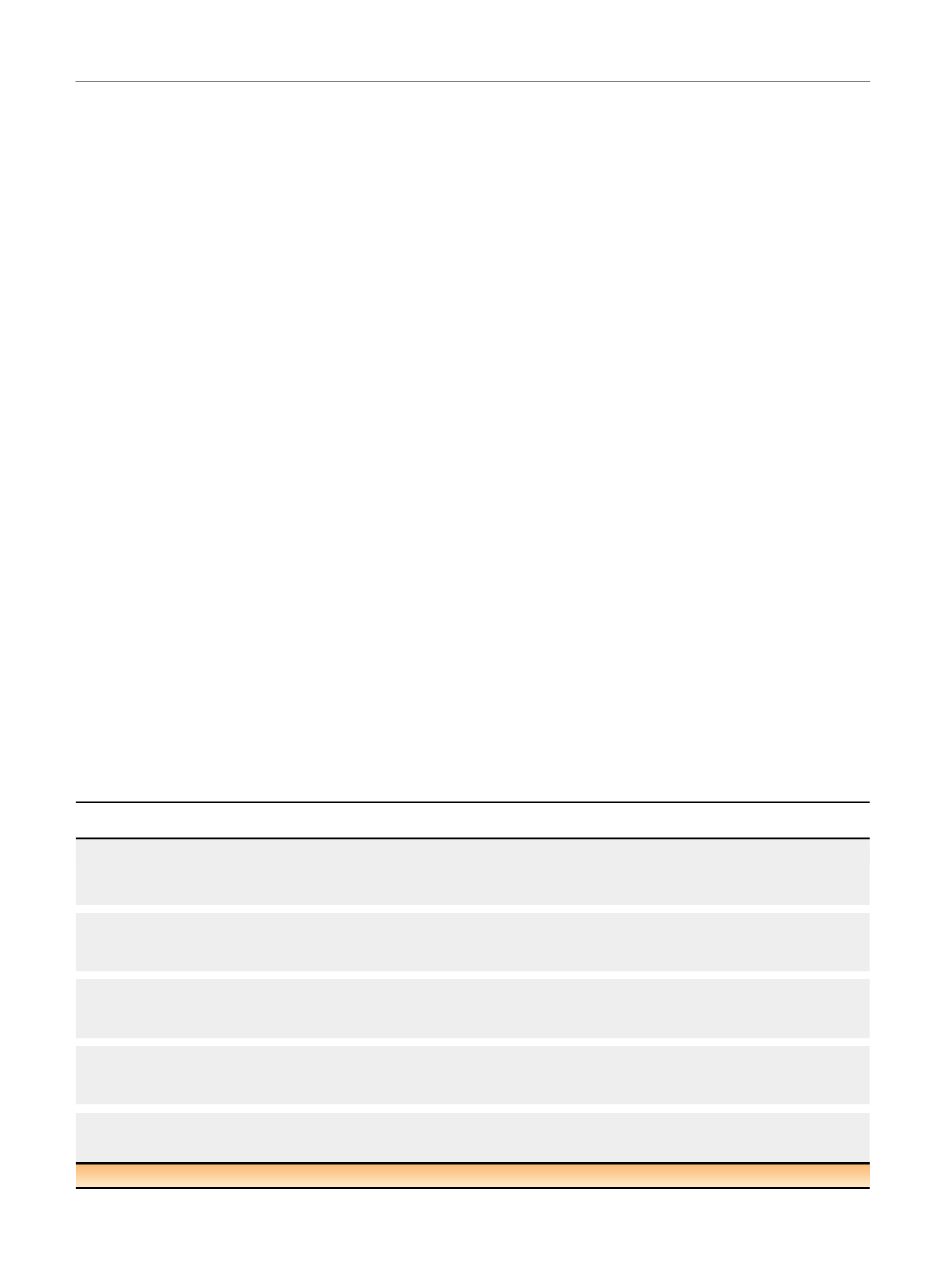
Table 3summarises the key issues identified
and strategies implemented to overcome these. This
intervention has since been refined in a number of RCTs
[24,26,31,32,44,50,52] ,and the final version of the QuinteT
Recruitment Intervention (QRI) is conducted in two phases.
Phase 1 aims to understand the trial recruitment process by
Table 3 – Issues identified in the ProtecT study and strategies to improve recruitment
[25]1. Organisation and presentation of study information
Treatments tended to be presented in a standard order: surgery, radiotherapy, and then active monitoring. Analysis showed that these options were not
presented equally. Recruiters were asked to present the treatments in a different order [(1) active monitoring, (2) surgery, and (3) radiotherapy] and to
describe their advantages and disadvantages.
2. Terminology used in study information
The term ‘‘trial’’ was sometimes interpreted as monitoring (‘‘try and see’’), so recruiters were asked to use ‘‘study’’ instead. Recruiters had tried to reassure
patients that there was a good 10-yr survival (‘‘the majority of men with prostate cancer will be alive 10 yr later’’). However, patients interpreted this to
suggest that they might die in 10 yr. It was recommended that recruiters present survival in terms of ‘‘most men with prostate cancer live long lives’’.
3. Specification and presentation of the nonradical arm
Recruiters often called the non-radical arm ‘‘watchful waiting,’’ but patients had interpreted this as ‘‘no treatment’’, where the disease would be
watched and the patient waited for death (‘‘watch while I die’’). This was renamed ‘‘active monitoring’’ and redefined to involve three monthly or six
monthly prostate specific antigen tests, with intervention if required or requested.
4. Presentation of randomisation and equipoise
Both recruiters and patients had difficulty with randomisation and equipoise. Recruiters were supported to feel comfortable discussing uncertainty
and explaining that patients were suitable for all three treatments. They were also advised to explain the rationale for randomisation and explain that
if the patient were uncertain, randomisation represented a way of resolving the dilemma of treatment choice.
5. Exploring patient preferences
Recruiters initially felt uncomfortable discussing patient preferences. Training emphasised that it was important to elicit and explore preferences,
particularly if these were not well founded in evidence (eg, rejecting radiotherapy because of a mistaken belief that it would lead to hair loss).
ProtecT = Prostate Testing for Cancer and Treatment trial.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 7 8 9 – 7 9 8
794
















