
for Statistical Computing, Vienna, Austria). The primary
objective of the study was to validate Decipher for
prediction of metastasis post-biopsy. Biopsy Grade Group
(1, 2–3 vs 4), clinical stage (
<
T2a vs T2a), and NCCN risk
groups (low, intermediate, and high) were treated as
categorical variables. Age at first-line treatment, pretreat-
ment PSA (log 2 transformed) and CAPRA were modeled as
continuous variables. In time-to-event analyses, event
times were defined as the time from biopsy to metastases
or date of last follow-up. Decipher was treated as a linear
variable since the likelihood ratio test showed that the
models including Decipher as quadratic or cubic terms were
not significantly different compared to the model including
Decipher as a linear variable (data not shown).
The performance of biopsy Decipher, CAPRA, and NCCN
risk categories were evaluated by their ability to: (1)
independently predict metastases using multivariable
(MVA) penalized Cox regression stratified by institution
using an adaptation of Firth’s approach. Due to the small
number of events and large number of predictors in MVA,
Firth’s penalized method was used for the identification of
the most prognostic risk factors to ensure the robustness of
the analyses and avoid overestimation of the resulting
hazard ratios (HRs)
[17], (2) discriminate metastasis risk
among patients using survival receiver operating charac-
teristic curves
[18] ,and (3) stratify metastatic risk using
cumulative incidence curves method of Fine and Gray, to
account for competing risks, death due to other causes
[19]. C-index of the combined models was estimated by
subjecting the model to bootstrapping with 1000 resamples
to correct for optimism. Confidence intervals for survival c-
indices were computed via the bootstrap. The c-indices
were considered statistically significant if the lower bound
of the 95% confidence interval (CI) exceeded 0.50. Five-year
endpoint was chosen for the survival area under the curve
calculation as it provides a clinically meaningful time-point.
In addition, 5-yr metastasis is the reported endpoint for the
commercial Decipher assay. Extension of the decision curve
analysis to survival data was employed to evaluate the net
benefit of Decipher, CAPRA, and Decipher plus CAPRAmodel
across clinically relevant threshold probabilities
[20]. In this
manuscript, we adhered to European Urology’s reporting
guidelines
[21].
3.
Results
3.1.
Patient characteristics
Demographic and clinical characteristics of the patients in
our study are provided in
Table 1. Median patient age at
first-line treatment was 64 yr. Median pretreatment PSA
was 7.0 ng/ml; 53% of patients had biopsy Grade Groups
2 and 3 and 53% had clinical stage T2a or higher. According
to NCCN classification, 54% and 32% were classified as
intermediate and high risk, respectively. Median follow-up
of censored patients was 6 yr. During the study follow-up,
34 patients developed metastases and 11 of these patients
died of PCa.
3.2.
Distribution of CAPRA and Decipher scores
Median CAPRA score was 4. Thirty Four (15%), 107 (46%),
and 66 (28%) patients were categorized as low, intermedi-
ate, and high risk by CAPRA, respectively (Supplementary
Fig. 1). Median Decipher score was 0.39. One hundred and
forty (60%), 42 (18%), and 53 (23%) of patients were
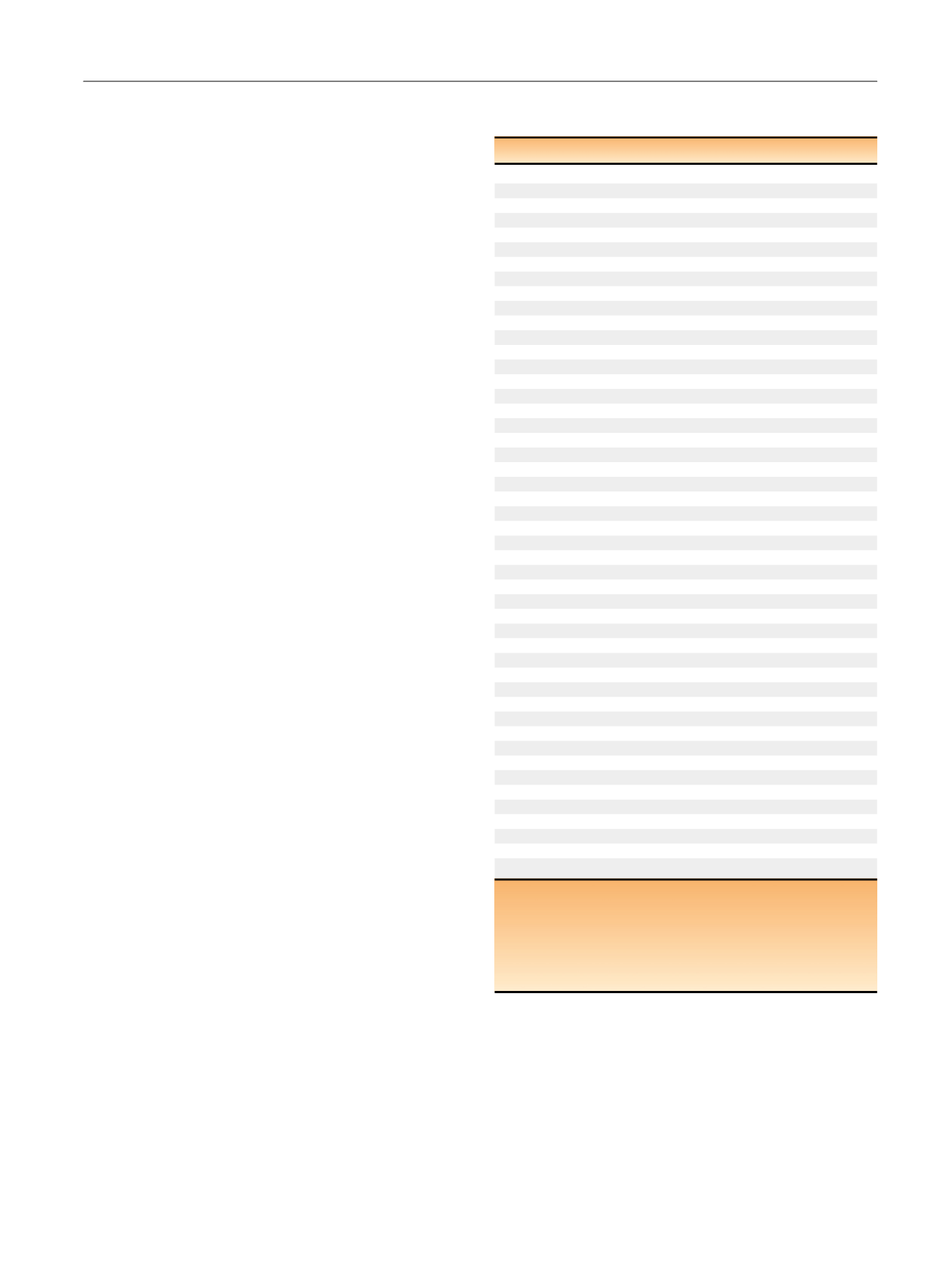
Table 1 – Demographic and clinical characteristics of analyzed
patients
Variables
Study cohort
No. patients (%)
235 (100)
Race
African American
32 (14)
Arabic
1 (0.43)
Asian
4 (1.7)
Caucasian
167 (71)
Hispanic
3 (1.3)
Other
28 (12)
Age at first line treatment (yr)
Median (IQR)
64 (58, 70)
PSA at first line
Median (IQR)
7 (4.6, 13.2)
Biopsy Grade Groups
Grade Group 1
44 (19)
Grade Group 2
65 (28)
Grade Group 3
59 (25)
Grade Group 4
32 (14)
Grade Group 5
35 (15)
Clinical stage
T1c
108 (46)
T2a
125 (53)
Unknown
2 (0.85)
NCCN risk groups
Low
25 (11)
Intermediate
128 (54)
High
75 (32)
Unknown
7 (3)
CAPRA risk groups
Low
34 (14)
Intermediate
107 (46)
High
66 (28)
Unknown
28 (12)
Median follow-up of censored patients’ yr
Median (IQR)
6 (4, 8)
First-line treatment
RP
105 (45)
RT ADT
130 (55)
Radiation therapy type
Brachy
1 (0.43)
CIMRT
8 (3.4)
EBRT
97 (41)
EBRT + Brachy
2 (0.85)
HIMRT
11 (4.7)
IMRT
11 (4.7)
Androgen deprivation therapy type
Antiandrogen therapy
1 (0.43)
Androgen deprivation therapy
19 (8.1)
Combined androgen blockade
91 (39)
ADT = androgen deprivation therapy; CAPRA = Cancer of the Prostate Risk
Assessment; CIMRT = conventionally intensity modulated radiation therapy;
EBRT = external beam radiation therapy; HIMRT = hypofractionated intensity
modulated radiation therapy; IMRT = intensity modulated radiation therapy;
IQR = interquartile range; NCCN = National Comprehensive Cancer Network;
PSA = prostate-specific antigen; RP = radical prostatectomy; RT = radiation
therapy.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 8 4 5 – 8 5 2
847
















