
reported in a recent study
[23] .Based on the findings in our
control group, we introduced a threshold to distinguish
physiologically low versus pathologically high AR-V7 levels
in mCRPC patients (0.6% of the ratio of AR-V7 transcripts
over total AR (AR-V7 plus AR-FL) transcripts). Using this
threshold, 18% of mCRPC patients exhibited high AR-V7
expression in our study.
The reported fraction of AR-V7
–
positive mCRPC patients
shows high variation, ranging between 11% and 68%
[8,11 – 15]. This is attributable to various causes, most importantly
the variety of methods used, including CTC-derived RNA- or
protein-based assays as well as different whole-blood assays.
However, the optimal method for determining AR-V7 status
using liquid biopsies has yet to be determined. While CTC-
based methods require detectable CTCs, whole blood
samples show tumor-independent AR-V7 expression, po-
tentially masking PCa-related AR-V7 expression to a certain
extent. Furthermore, the variation in AR-V7 detection rates
may be attributable to the heterogeneity of patient cohorts.
In our study, AR-V7 positivity ranged from 0% to 30%
corresponding to a range of zero to three prior lines of
systemic treatment for mCRPC, comprising taxane chemo-
therapy and AR-directed agents. Keeping in mind that AR-V7
positivity becomes more frequent in patients pretreated
with AR inhibitors
[8]and taxane pretreatment might re-
establish sensitivity to AR-directed agents by AR-V7 rever-
sion
[24 – 26] ,the number and sequence of prior treatment
regimens may have an important impact on AR-V7 status.
Our study results are in line with the current paradigm
considering AR-V7 expression as a predictor for nonre-
sponse to next-generation AR-directed therapy. However,
this paradigm has recently been challenged
[11,27]. Stei-
nestel et al
[11]described one patient who showed a PSA
response to abiraterone despite CTC positivity for AR-V7
mRNA. Likewise, Bernemann et al
[27]from the same group
conducted a retrospective study in which PSA response to
abiraterone or enzalutamide was assessed in 21 patients
with CTCs positive for AR-V7 mRNA. In their cohort, four
patients (19%) achieved a PSA decline 50%. One potential
explanation is that AR-V7
–
positive patients achieving a PSA
response might lack AR-V7 protein expression with correct
nuclear localization
[12] .Moreover, CTCs might express
AR-V7 mRNA at physiologically low levels in relation to AR-
FL, causing a positive test result without leading to
treatment resistance
[10].
In our cohort, we also observed three patients with high
AR-V7 levels who had a close to 50% PSA decline (43%, 46%,
and 48%), all of whom were treated with abiraterone.
However, these patients did not experience prolonged
benefit from their treatment. Two of the patients developed
clinical progression within 3 mo, and the third patient
experienced clinical progression after 4 mo and died after
6 mo.
A strength of our approach is the applicability in a clinical
routine setting. PAXgene tubes used for blood draw allow for
RNA stabilization at room temperature for approximately 4 d,
and storage at 80 C over long time periods. Furthermore, it
has been shown that digital PCR is reproducible across
laboratories
[28]with greater precision, better day-to-day
reproducibility, and similar sensitivity
[20_TD$DIFF]
compared to quanti-
tative real-time PCR.
Our study has the following limitations. First, the
retrospective design and patient enrolment at a single
institution limit the generalizability of our results. Second,
the number of AR-V7 high patients onwhich our findings are
based (
n
= 15) is relatively low. Third, among AR-V7 low
patients, 50% (31 of 62) failed to show a PSA response,
meaning that resistance mechanisms other than AR-V7 are
contributing to therapy failure and are not captured by AR-
V7 testing.
5.
Conclusions
We established a robust liquid profiling approach for direct
quantification of AR-V7 mRNA levels in peripheral whole
blood. In patients undergoing treatment with abiraterone
or enzalutamide, high AR-V7 levels predicted resistance,
with no PSA response and shorter PSA-PFS, clinical PFS,
and OS. These results support AR-V7 as a predictive
biomarker for nonresponse to next-generation AR-directed
therapy. Nevertheless, the optimal method for determining
AR-V7 status has yet to be determined. Moreover, a
randomized controlled trial is urgently needed to deter-
mine the clinical utility of AR-V7 as a resistance marker
and quantify the survival benefit of AR-V7
–
guided therapy
selection.
Author contributions:
Matthias M. Heck had full access to all the data in
the study and takes responsibility for the integrity of the data and the
accuracy of the data analysis.
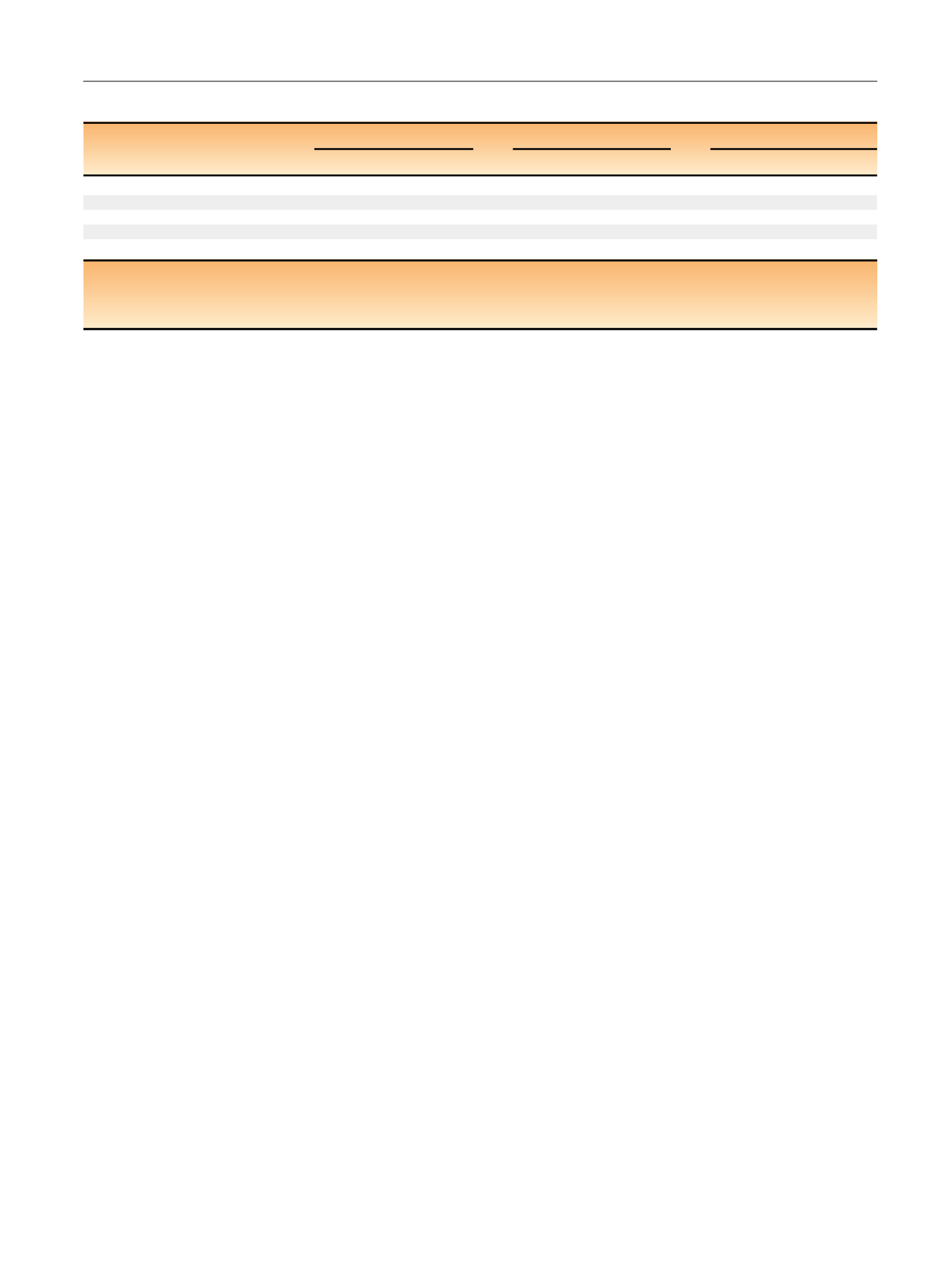
Table 3
–
Multivariable Cox regression analyses
aVariable
PSA-PFS
Clinical PFS
Overall survival
HR (95% CI)
p
value
HR (95% CI)
p
value
HR (95% CI)
p
value
AR-V7 (high vs low)
6.99 (2.36
–
20.7)
<
0.001
2.33 (1.12
–
4.86)
0.02
2.97 (1.39
–
6.33)
0.005
Abi/Enza pretreatment (yes vs no)
1.54 (0.72
–
3.27)
0.26
1.27 (0.65
–
2.46)
0.48
1.6 (0.72
–
3.57)
0.25
ECOG (0, 1, or 2)
1.81 (1.02
–
3.21)
0.04
1.73 (1.11
–
2.72)
0.02
2.46 (1.47
–
4.11)
<
0.001
Visceral metastases (yes vs no)
2.03 (1.05
–
3.94)
0.04
2.27 (1.28
–
4.05)
0.005
1.13 (0.6
–
2.12)
0.71
PSA (continuous, units of 100 ng/ml)
0.99 (0.95
–
1.03)
0.62
0.99 (0.96
–
1.02)
0.47
1 (0.97
–
1.03)
0.79
a
For the outcomes prostate-specific antigen progression-free survival (PSA-PFS), clinical PFS, and overall survival, one multivariable model for association of the
covariates AR-V7, prior treatment with abiraterone (Abi) or enzalutamide (Enza), Eastern Cooperative Oncology Group (ECOG) performance status, presence of
visceral metastases, and serum PSA levels with the outcome variable was created.
HR = hazard ratio; CI = confidence interval,
E U R O P E A N U R O L O GY 7 2 ( 2 0 17 ) 8 2 8
–
8 3 4
833
















