
3.4.
Secondary survival analyses
Associations between current postdiagnostic aspirin and
improved survival did not hold for cases diagnosed in the
PSA era
( Table 3). Results were similar when PC mortality
was the outcome (Supplementary
Table 2).
PC diagnosis was not strongly related to change in
aspirin use. Among cases diagnosed in 1995–1997 (mid
follow-up), 69% of nonusers started aspirin and 29% of users
stopped. For participants not diagnosed during this time,
the corresponding numbers were 48% and 24%. Prediag-
nostic and postdiagnostic aspirin were moderately corre-
lated (
r
= 0.39,
p
<
0.0001).
4.
Discussion
In the risk analysis, past and current prediagnostic aspirinuse
among men initially free of diagnosed cancer was associated
with significantly lower lethal PC incidence. Current use was
associated with lower overall mortality. In the survival
analysis, postdiagnostic aspirin use among men diagnosed
with nonlethal PC was associated with prolonged survival.
Many associations were stronger before PSA testing was
common. After PSA testing became widespread, diagnosis
occurred 11 yr earlier in disease progression on average
[25]; thus, ‘‘postdiagnostic’’ aspirin in the PSA era was
probably comparable to an earlier point in disease
progression in the pre-PSA era. We speculate that stronger
associations among men diagnosed before PSA testing may
indicate that the benefit of aspirin occurs later in disease
progression. This is consistent with our finding that aspirin
is not associated with initial diagnosis; progression to
lethality occurs later. In the risk analysis, aspirin also
appeared to be more protective against lethality in the PSA
era, again perhaps reflecting exposure at a later point in
disease progression than for screen-detected cancers. It is
also possible that the different associations in the pre-PSA
and PSA eras were partially due to changing patterns of
aspirin use among participants. In the pre-PSA era, aspirin
usage was increasing. Thus, because we stopped exposure
at prostate cancer diagnosis while continuing update for
non-cases, this may have lead to an overestimate of the
apparent protective effect of aspirin. However, in the PSA
era, aspirin use was decreasing, which would cause an
underestimate of aspirin’s protective effect.
Past postdiagnostic aspirin use was associated with
poorer survival and past use was associated with higher
overall mortality in the risk analysis. The latter association
may be due to sicker men stopping aspirin use. Confounding
by indication is possible despite efforts to adjust for
confounders; men may stop aspirin use as their disease
progresses. Conversely, healthier men may continue to take
aspirin. These tendencies would probably exaggerate the
apparent benefit. In addition, health-conscious men might
take aspirin for primary prevention, but men at higher risk
of cardiovascular disease may also take it, so confounding
by indication could have effects in either direction.
No significant effects were observed in the underpow-
ered ITT analyses, with only 20 lethal events during the 5-yr
randomization period. However, the HR of 0.69 was similar
to that in the primary risk analysis.
Several previous studies also suggest that regular aspirin
is associated with reduced PC progression. Among
1499 men diagnosed with high-risk PC, daily postdiagnostic
aspirin was associated with lower PC mortality, with no
apparent protection from prediagnostic aspirin
[26]. In a
retrospective analysis of 5955 patients who received local
treatment, aspirin was associated with lower PC mortality
[27]. By contrast, in another retrospective study among
11 779 men diagnosed with nonlethal PC, postdiagnostic
aspirin was associated with greater PC-specific and overall
mortality
[8] .However, aspirin use was based on electronic
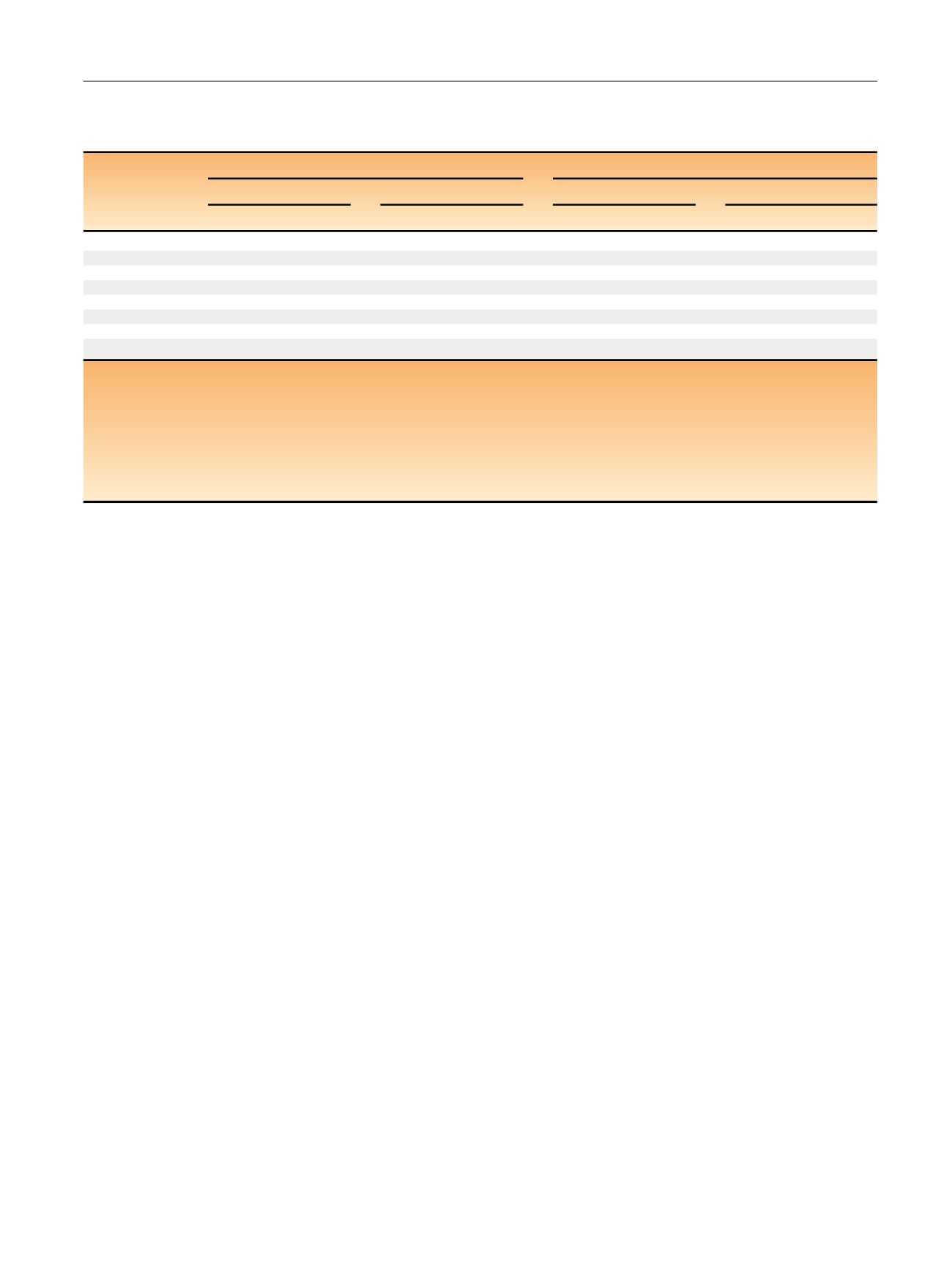
Table 6 – Survival analysis. Regular postdiagnosis aspirin use
a and survival to lethal prostate cancer
b and overall mortality among prostate
cancer patients diagnosed with nonmetastatic disease in the Physicians’ Health Study: analyses stratified by diagnosis before or during the
PSA era
c (n
= 3277 patients)
Before the PSA era (
n
= 665 PC diagnoses)
During the PSA era (
n
= 2597 PC diagnoses)
Lethal prostate cancer
Overall mortality
Lethal prostate cancer
Overall mortality
Cases
MHR (95% CI)
dCases
MHR (95% CI)
dCases
MHR (95% CI)
dCases
MHR (95% CI)
dAspirin use
Never use
37
1.00 (reference)
91
1.00 (reference)
50
1.00 (reference)
162
1.00 (reference)
Past use
63
0.91 (0.54–1.53)
215
1.03 (0.76–1.40)
67
2.05 (1.35–3.12)
211
1.41 (1.12–1.77)
Current use
70
0.50 (0.31–0.80)
210
0.54 (0.40–0.73)
120
0.73 (0.51–1.05)
439
0.77 (0.64–0.94)
Duration
Never
37
1.00 (reference)
91
1.00 (reference)
50
1.00 (reference)
162
1.00 (reference)
Current, 1–4 yr
32
0.54 (0.29–1.02)
60
0.49 (0.32–0.75)
67
0.72 (0.46–1.11)
175
0.70 (0.55–0.90)
Current, 5 yr
38
0.43 (0.23–0.82)
150
0.62 (0.43–0.90)
53
0.74 (0.46–1.19)
264
0.84 (0.67–1.05)
PSA = prostate-specific antigen; PC = prostate cancer; MHR = multivariate hazard ratio; CI = confidence interval.
a
Regular aspirin use is defined as taking
>
3 tablets/wk for at least 1 yr. The postdiagnosis survival analysis value is updated until lethality or overall mortality.
b
Lethal prostate cancer is defined as tumor metastases to bones or other organs or death if the cause of death was prostate cancer.
c
For survival analysis the pre-PSA era only includes prostate cancer cases diagnosed before 1992. The PSA era only includes prostate cancer cases diagnosed
1992 or after.
d
Multivariate models adjusted for age at diagnosis (years; continuous), calendar year of diagnosis (continuous), race (white, non-white/missing), Charlson
comorbidity index (0, 1–2,
>
2) body mass index (kg/m
2
; continuous), smoking status (current, past [quit within 10 yr], never/remote [quit
>
10 yr ago], PSA
level at diagnosis (ng/ml;
<
10, 10–20,
>
20, missing), Gleason score sum ( 6, 7, 8–10, missing), clinical stage (T1–2, T3, T4/N1, missing), and primary
treatment (radical prostatectomy, radiotherapy, other/none).
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 8 2 1 – 8 2 7
825
















