
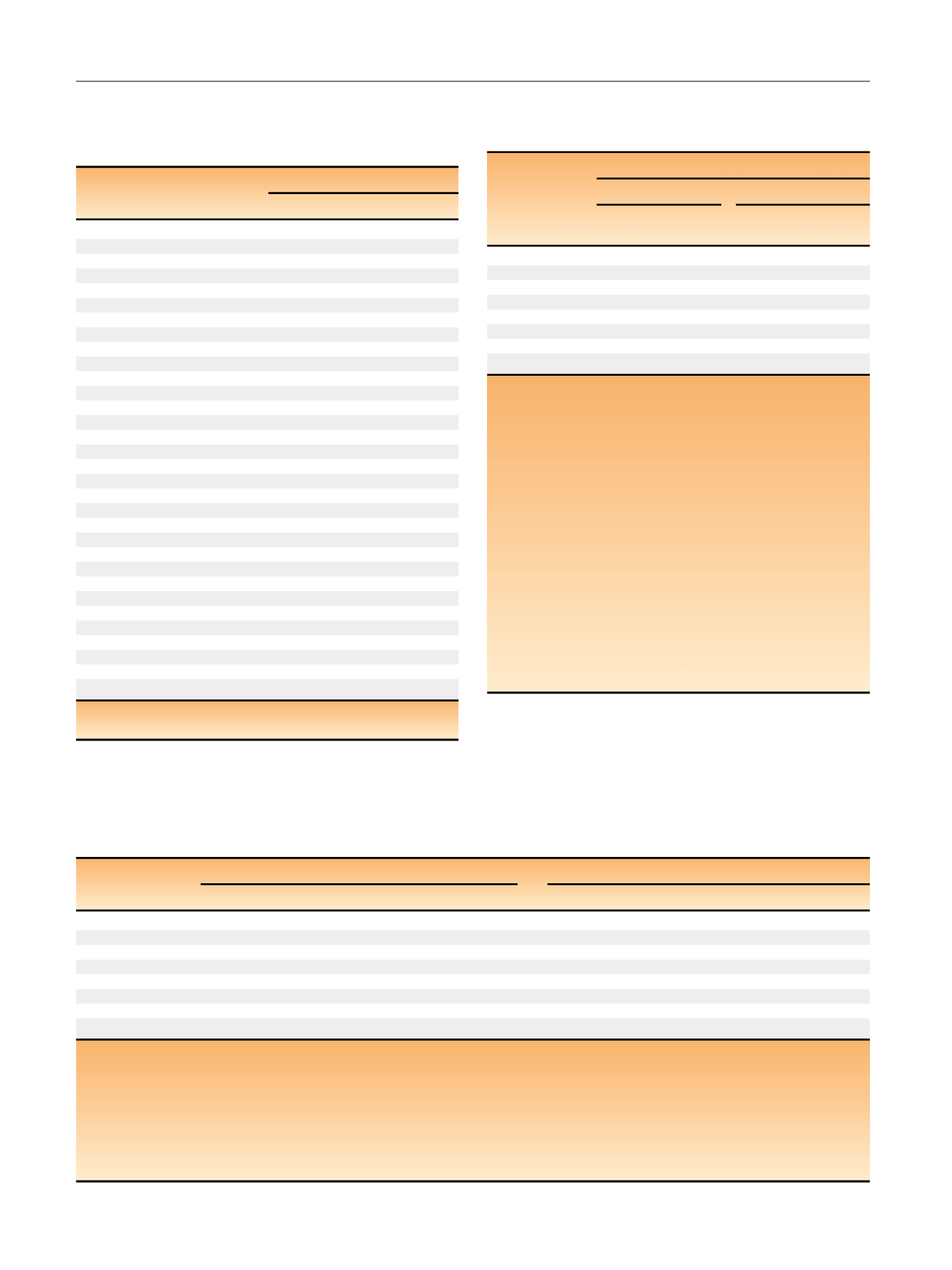
Table 3 – At-diagnosis characteristics for the survival analysis
according to regular aspirin use at prostate cancer diagnosis
among all men diagnosed with nonmetastatic prostate cancer in
the Physicians’ Health Study
At-diagnosis characteristics
Regular aspirin use at diagnosis
Yes (
>
3 d/wk)
No ( 3 d/w)
2083
1194
Age (yr)
71.2
71.9
Body mass index (kg/m
2
)
25.6
25.2
Height (cm)
179
179
Race
White
93
89
Non-white
7
11
Smoking status
Never/quit
>
10 yr ago
48
49
Past, quit within 10 yr
48
47
Current
4
4
Medical history
Hypertension
59
52
Diabetes
8
7
Prostate-specific antigen
<
10 ng/ml
41
42
10–20 ng/ml
12
12
>
20 ng/ml
7
6
Gleason score sum
6
49
49
7
22
22
8–10
10
12
Clinical stage
T1
35
34
T2
41
42
T3
5
4
T4/N1
1
1
Primary treatment
Radical prostatectomy
36
37
Radiotherapy
28
27
Other/bone
64
64
Year of diagnosis
1999
1998
Results are presented as the age-adjusted mean for continuous variables
and as the percentage frequency for categorical variables.
Table 5 – Risk analysis. Regular prediagnosis aspirin use
a and risk
of lethal prostate cancer
b , c for prostate cancer cases diagnosed
before and during the PSA era
dLethal prostate cancer
Before the PSA era
During the PSA era
Cases
MHR
(95% CI)
eCases
MHR
(95% CI)
eAspirin use
Never use
69 1.00 (reference)
16 1.00 (reference)
Past use
33 0.31 (0.20–0.48)
91 0.99 (0.58–1.69)
Current use
131 0.59 (0.43–0.81)
162 1.01 (0.60–1.69)
Duration
Never
69 1.00 (reference)
16 1.00 (reference)
Current, 1–4 yr
30 0.62 (0.39–0.97)
8 1.05 (0.44–1.49)
Current, 5 yr
101 0.56 (0.39–0.79)
154 1.06 (0.63–1.80)
PSA = prostate-specific antigen; MHR = multivariate hazard ratio;
CI = confidence interval.
a
Regular aspirin use is defined as taking
>
3 tablets/wk for at least 1 yr,
with risk analysis values updated until prostate cancer diagnosis.
b
Lethal prostate cancer is defined as tumor metastases to bones or other
organs or death if the cause of death was prostate cancer. Risk outcomes
are defined as time from 1981/82 baseline until outcome (metastasis or
death, whichever came occurred first).
c
Whether an event was included in pre-PSA or PSA era analyses
depended on the date of initial prostate cancer diagnosis. Most men who
died in the risk analysis were not diagnosed with prostate cancer, so we
could not analyze the risk of overall mortality according to timing of
diagnosis.
d
For the pre-PSA era, lethal prostate cancer was only considered an event
if patients were initially diagnosed before 1992. For the PSA era, lethal
prostate cancer was only considered an event if patients were initially
diagnosed in 1992 or thereafter.
e
Multivariate models adjusted for age (years; continuous), race (white,
non-white/missing), body mass index (kg/m
2
; continuous), height
(m; continuous), smoking status (current, past [quit within 10 yr], never/
remote [quit
>
10 yr ago]), hypertension (yes, no), and diabetes (yes, no).
Table 4 – Survival analysis. Regular postdiagnosis aspirin use
a and survival to lethal prostate cancer
b and overall mortality among prostate
cancer patients diagnosed with nonmetastatic disease in the Physicians’ Health Study (
n
= 3277 patients)
Lethal prostate cancer
Overall mortality
Cases
PY
AAHR (95% CI)
MHR (95% CI)
cCases
PY
AAHR (95% CI)
MHR (95% CI)
cAspirin use
Never use
87
7105 1.00 (reference)
1.00 (reference)
253
7105 1.00 (reference)
1.00 (reference)
Past use
130
6572 1.42 (1.06–1.91)
1.50 (1.10–2.05)
426
6572 1.28 (1.08–1.52)
1.28 (1.08–1.53)
Current use
190
27 971 0.60 (0.46–1.77)
0.68 (0.52–0.90)
649
27971 0.68 (0.58–0.79)
0.72 (0.61–0.84)
Duration
Never
87
7105 1.00 (reference)
1.00 (reference)
253
7105 1.00 (reference)
1.00 (reference)
Current, 1–4 yr
99
13 240 0.61 (0.44–0.84)
0.70 (0.50–0.97)
235
13240 0.61 (0.50–0.74)
0.62 (0.51–0.76)
Current, 5 yr
91
14 731 0.55 (0.39–0.78)
0.66 (0.46–0.95)
414
14731 0.73 (0.61–0.87)
0.80 (0.67–0.97)
PY = person-years; AAHR = age-adjusted hazard ratio; CI = confidence interval; MHR = multivariate hazard ratio.
a
Regular postdiagnosis aspirin use is defined as taking
>
3 tablets/wk for at least 1 yr. The postdiagnosis survival analysis value is updated until lethality or
overall mortality.
b
Lethal prostate cancer is defined as tumor metastases to bones or other organs or death if the cause of death was prostate cancer. The date was taken for
whichever outcome occurred first. Survival analysis outcomes are defined as time from prostate cancer diagnosis until outcome.
c
Multivariate models adjusted for age at diagnosis (years; continuous), calendar year of diagnosis (continuous), race (white, non-white/missing), Charlson
comorbidity index (0, 1–2,
>
2) body mass index (kg/m
2
; continuous), smoking status (current, past [quit within 10 yr], never/remote [quit
>
10 yr ago], PSA
level at diagnosis (ng/ml;
<
10, 10–20,
>
20, missing), Gleason score sum ( 6, 7, 8–10, missing), clinical stage (T1–2, T3, T4/N1, missing), and primary
treatment (radical prostatectomy, radiotherapy, other/none).
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 8 2 1 – 8 2 7
824
















