
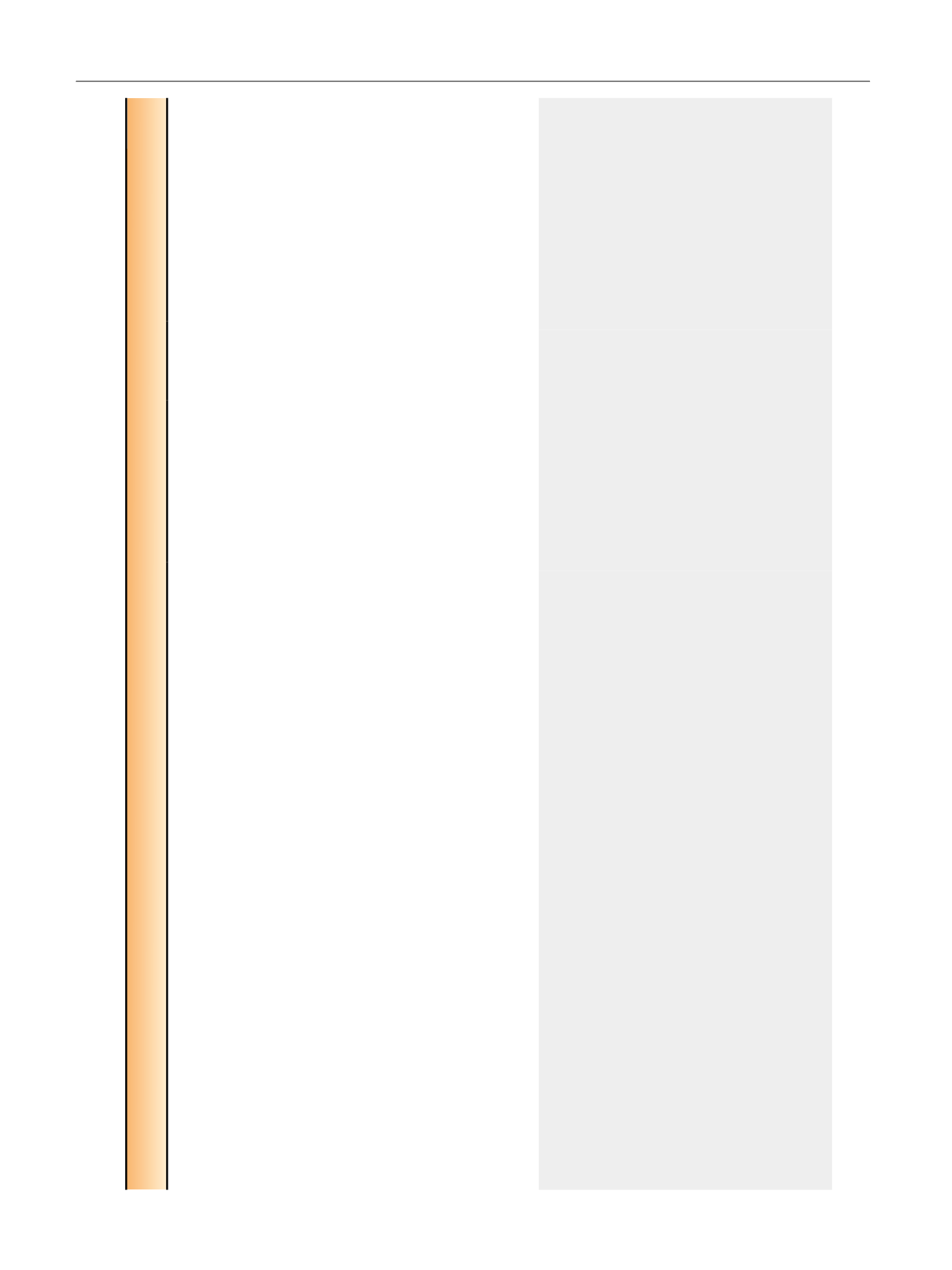
Table 3 – Studies comparing cost of proton beam therapy and IMRT
Study
Patients, no.
Type of
study
Data source
Comparison Cost definition Costs included (direct vs
indirect)
Perspective Main findings including comment on
risk of bias
Studies from the payer’s perspective
Konski (2007)
[45]
NA
Cost
modeling
Data from literature
and patient interviews
Proton versus
IMRT
Costs modeled
in decision tree
analyses
(Markov model)
Direct costs
Payer’s
(Medicare)
perspective
70 yr old (15-yr cost)
Proton cost: $63 511 (2005)
IMRT cost: $36 808 (2005)
Difference: $26 703 (2005)
ICER: $63 578/QALY
60 yr old (15-yr cost)
Proton cost: $64 989 (2005)
IMRT cost: $39 355 (2005)
Difference: $25 634 (2005)
ICER: $55 726/QALY
Model calculated cost effectiveness based
on a third-party payer (Medicare) and did
not include upfront costs or yearly
operational costs.
Sensitivity analyses included how many
years the model was run, patient’s age,
probability of freedom from biochemical
failure for proton and IMRT, utility of
patients treated with salvage hormone
therapy, and treatment costs.
Risk of bias high due to uncertainty of the
data abstracted from the literature.
Yu (2013)
[4]553 Proton
27 094 IMRT
Retrospective
cohort study
Retrospective study
of Medicare beneficiaries
from 2008 to 2009
(Medicare data)
Proton versus
IMRT
Medicare
payments
Direct costs; did not account
for indirect costs, such as
long travel distances for
proton patients
Payer
Median Medicare reimbursement
Proton: $32 428
IMRT (matched group): $18 575
Difference: $13 853
Cost of Proton and IMRT was calculated
using the sum of Medicare reimbursements
for all outpatient and physician claims with
HCPCS codes indicative of radiotherapy,
including treatment planning,
management, and delivery, in the 3 mo
following initiation of radiation.
No adjustments for inflation, although only
a 2-yr study.
Used Mahalanobis matching to account for
known confounders; could not use
propensity score or instrumental variable
analysis due to small proton numbers.
Risk of bias moderate as residual
confounding may be present.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 7 1 2 – 7 3 5
730
















