
2.2.6.
Lymph node dissection
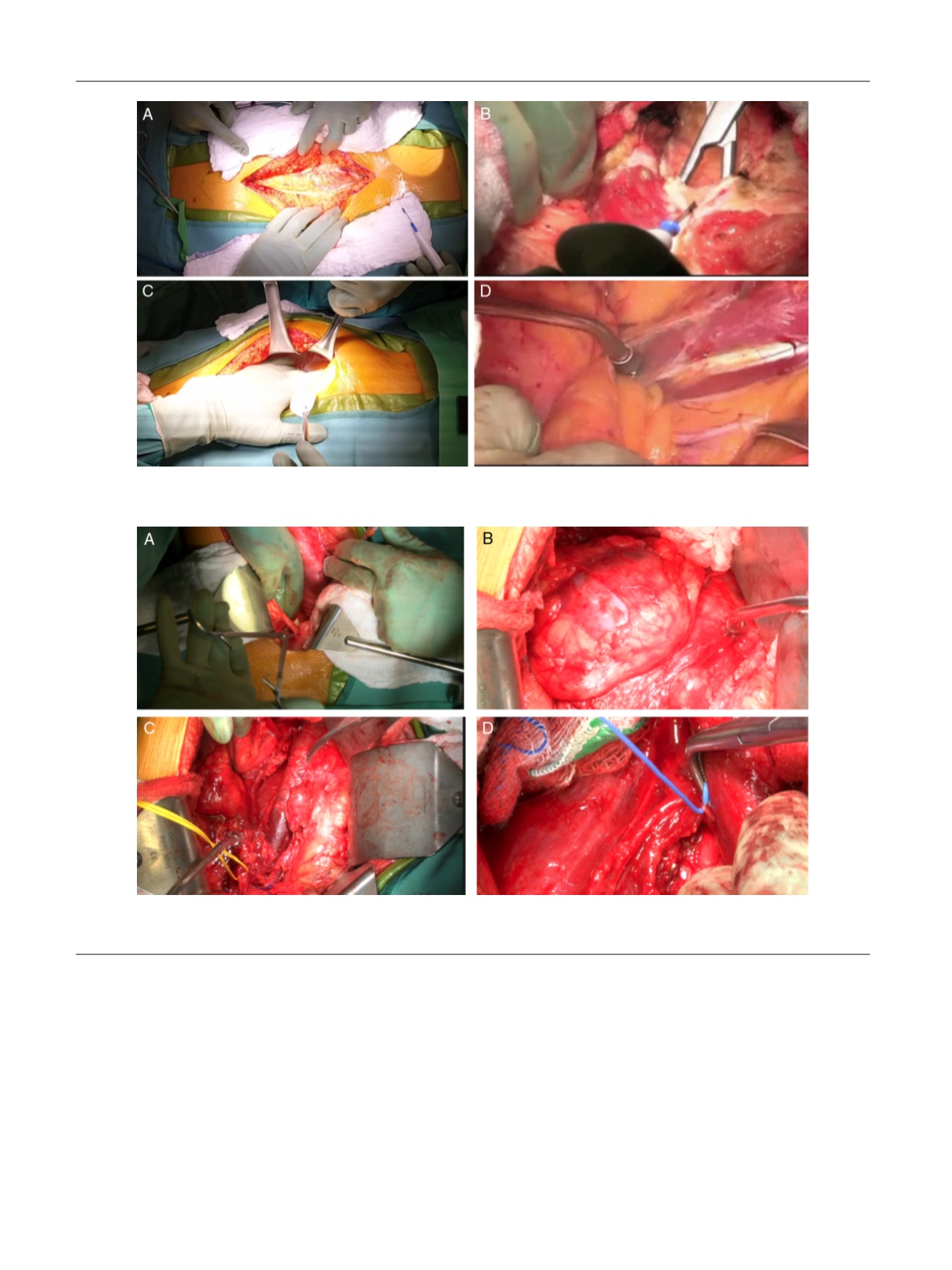
Prospective identification of the sympathetic post-ganglionic nerves is
performed first
( Fig. 2D). Then dissection of the ipsilateral gonadal
vessels, interaortocaval dissection, and contralateral vessel exposure and
mobilization with retrocaval or paraaortic nodal dissection are carried
out in a typical fashion. A left-sided RPLND is performed in an identical
manner
( Fig. 3A,B), with the EP plane developed from the left side. The
inferior mesenteric artery (IMA) occasionally acts as a tether for a left-
sided approach when a full bilateral template or resection of a mass
below the IMA necessitates dissection here. In this case, the IMA can
usually be skeletonized to achieve the needed mobility without
requiring ligation. Care must be taken to avoid damage to the nerves
as they coalesce into the superior hypogastric plexus in this area.
2.2.7.
Closure
The peritoneal sac is released and inspected for peritoneotomies
(
Fig. 3 C). Peritoneotomies are closed using 3-0 vicryl or 3-0 chromic
sutures
( Fig. 3 D).
In the majority of cases no drains are placed; if the mass is very large
or if warranted by concomitant extirpative procedures a closed bulb
suction drain is placed in the retroperitoneum. The incision is closed in a
typical fashion. When an epidural catheter is not present, para-incisional
[(Fig._2)TD$FIG]
Fig. 2 – (A) Ureteral identification. (B) Full mobilization of the kidney from the peritoneal sac. (C) Visualization of the great vessels. (D) Prospective
nerve-sparing step.
[(Fig._1)TD$FIG]
Fig. 1 – (A) Midline incision. (B) Incision of the posterior rectus. (C) Development of the extraperitoneal space. (D) Development of the retroperitoneal
space.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 8 1 4 – 8 2 0
816
















